 全世界每年大约有300万人遭受自发性脑内出血(ICH)。在大多数患者中,ICH是由脑小血管疾病(SVD)引起的,影响到大脑的小穿孔血管。ICH的存活者有复发中风(包括复发的ICH和缺血性中风)和其他血管事件的高风险。在ICH后数天至数月进行的脑磁共振成像(MRI)中,11%-41%的患者存在弥散加权成像阳性(DWI+)病变。
全世界每年大约有300万人遭受自发性脑内出血(ICH)。在大多数患者中,ICH是由脑小血管疾病(SVD)引起的,影响到大脑的小穿孔血管。ICH的存活者有复发中风(包括复发的ICH和缺血性中风)和其他血管事件的高风险。在ICH后数天至数月进行的脑磁共振成像(MRI)中,11%-41%的患者存在弥散加权成像阳性(DWI+)病变。
最近一项调查DWI+病变与ICH各种亚型之间关系的荟萃分析显示,ICH后90天内DWI+病变的发生率平均为20%。此外,在所有ICH中,DWI+病变与先前的ICH和脑MRI上其他SVD生物标志物有关。DWI+病变是否能预测ICH后的临床事件仍不确定。
在一些研究中,不良的功能结局(由ICH后3个月的改良Rankin量表评分评估)与DWI+病变的存在有关,但与其他研究无关。一项针对97名患者的研究发现,在3.5年的中位随访期内,ICH后5天出现DWI+病变与缺血性卒中以及缺血性卒中、复发性ICH和血管性死亡的复合风险较高有关。
然而,另一项针对466名ICH患者的研究发现,DWI+病变的存在与缺血性卒中的高风险有关,但与复发ICH无关。
因此,荷兰Radbound University的Kim Wiegertjes等人,通过对REstart或STop抗血栓随机试验(RESTART)的事后探索性亚组分析,研究抗血栓相关ICH幸存者中DWI+病变的存在是否与复发卒中有关。
方法 REstart or STop Antithrombotics Randomised Trial (RESTART)评估了ICH后重新开始与避免抗血小板治疗对主要血管事件的影响,时间长达5年。我们在掩盖结果和抗血小板使用的情况下,对随机化前做的MRI的DWI序列进行评分,看是否存在DWI+病变。最后使用Cox比例危害回归模型来量化关联。
他们发现:在RESTART的537名参与者中,247人(中位数(IQR)年龄为75.7(69.6-81.1)岁;170名男性(68.8%);120人开始与127人避免使用抗血小板治疗)在ICH后的中位数57天(IQR 19-103)有脑MRI序列,其中73人(30%)有一个或多个DWI+病灶。
在2年(1-3)的中位随访期间,18名参与者有复发性ICH,21名参与者有缺血性中风。DWI+病变的存在与所有卒中(调整HR为2.2(95%CI为1.1至4.2))和复发性ICH(4.8(95%CI为1.8至13.2))相关,但与缺血性卒中(0.9(95%CI为0.3至2.5))无关。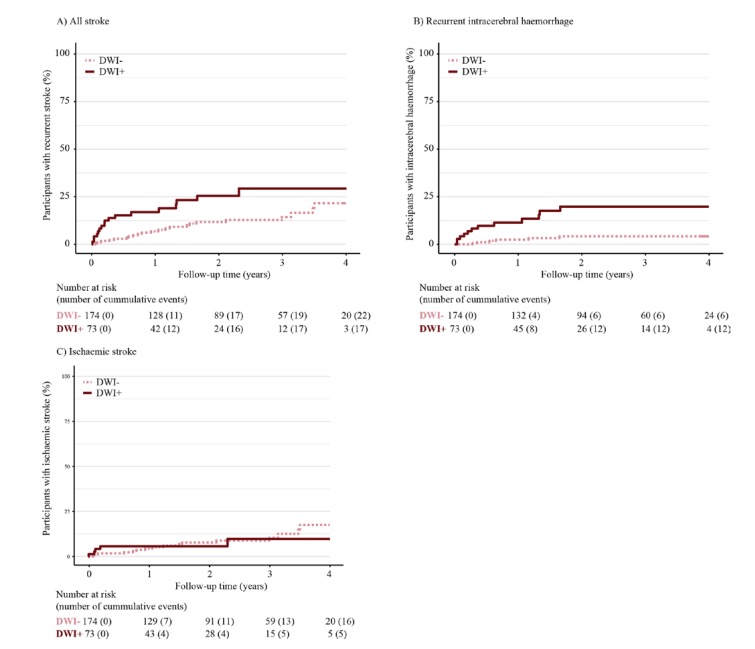
DWI+病变的存在没有改变抗血小板治疗对复发卒中综合结果的影响。
这个研究的重要意义在于发现了:ICH存活者的DWI+病变存在与复发性ICH有关,但与缺血性卒中无关。并没有发现DWI+病变的存在会改变抗血小板治疗对ICH后复发卒中的影响。这些发现为DWI+病变的意义提供了一个新的视角,它可能是与复发性ICH相关的微血管机制的标志物。
原文出处:
Wiegertjes K, Dinsmore L, Drever J, et al
Diffusion-weighted imaging lesions and risk of recurrent stroke after intracerebral haemorrhage
Journal of Neurology, Neurosurgery & Psychiatry Published Online First: 08 June 2021. doi: 10.1136/jnnp-2021-326116
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#复发性#
36
#DWI#
43
#自发性脑出血#
45
#自发性#
36
加强技术革新
57