TCT 2020|王盛教授点评:应用替西罗莫司药物的外膜递送系统为BTK的治疗提供新思路
2020-11-06 《门诊》杂志 门诊新视野
目前,针对膝下血管的血管内治疗的长期疗效令人担忧,其原因可能是由于药物的腔内应用,不能穿透重重组织和小管腔动脉内的斑块负荷。
目前,针对膝下血管的血管内治疗的长期疗效令人担忧,其原因可能是由于药物的腔内应用,不能穿透重重组织和小管腔动脉内的斑块负荷。美国纽约当地时间10月18日,第32届美国经导管心血管治疗学术会议虚拟会议(TCT 2020)期间,Ehrin Armstrong教授公布了TANGO研究6个月随访结果。为加深各位读者对TANGO研究的了解,《门诊》杂志特邀首都医科大学附属北京安贞医院王盛教授对本次研究进行了精彩的点评。
专家点评
TANGO是TCT 2020上发布的比较重磅的LBCT研究,意在评估Bullfrog Micro-Infusion外膜递送系统应用替西罗莫司治疗膝下动脉病变的效果,6个月的随访结果令人满意。膝下动脉病变多为长段闭塞、多节段病变,且动脉管径细小,一直是临床治疗的难题。TANGO研究聚焦膝下动脉病变,为膝下动脉病变治疗提供了新的策略和思路。除此之外,相较于既往的临床研究,TANGO研究还具有以下两个特点。
1、独特的药物递送系统:不同于当前的DCB、DES的给药方式,TANGO研究使用了新兴的Bullfrog Micro-Infusion外膜递送系统,通过注射针头直接向血管壁内给药,达到垂直定向的给药目的;使得药物能够直达血管内膜、中膜甚至外膜,避免了药物在血液中的流失,提高了药物的安全性和使用效率,同时大大降低了严重钙化斑块对药物扩散的不利影响。此外,该药物递送系统在治疗股腘动脉病变的临床研究中表现不俗,而TANGO研究证实了其在膝下动脉病变的治疗中也能取得不错的效果。因此,我认为该药物递送系统可能会在未来外周动脉疾病的治疗中有一定的使用价值。
2、独特的药物选择:该研究使用的药物是替西罗莫司,而不是下肢动脉载药器具常用的紫杉醇。事实上,外周动脉疾病中药物的使用经历了莫司类药物到紫杉醇药物的多次摸索;而在紫杉醇药物安全性备受争议的当下,该研究重启替西罗莫司在外周动脉疾病的应用,并取得了不错的效果。这也提示广大血管外科医师在临床工作中发散思维,不要拘泥于当前的药物或器具,大胆探索,寻找和创新更适合外周动脉疾病的药物和器具。
需要注意的是,TANGO研究令人满意的结果并不仅是替西罗莫司的功劳,还归功于独特的药物递送系统避免了钙化和血管弹性回缩的影响。因此,对于替西罗莫司的长期疗效,仍需要更多、更大规模、更长随访的研究加以证实。当然,不管膝上或膝下动脉病变的治疗都需要临床医师充分重视血管准备,再配合疗效更加优异的药物和递送系统,治疗复杂下肢动脉病变势如破竹。
TANGO:一项血管外膜应用替西罗莫司药物 剂量递增改善BTK治疗预后的随机对照研究
研究目标
评估Bullfrog Micro-Infusion 装置外膜沉积替西罗莫司剂量递增在减少膝下(BTK)动脉血运重建术后新生内膜增生和靶病变失败方面6个月有效性和安全性。
研究方法
该研究为前瞻性、多中心、随机、双盲、剂量递增研究,共纳入了61例接受血管内血运重建的患者,BTK病变数量≥1。符合条件的患者的Rutherford分级为 3~5级,并正在接受≥1种血管内治疗(不包括其他基于药物的干预措施)。动脉血运重建完成后给予治疗,分为对照组(生理盐水;病变长度0.25~0.50 mL/cm),低剂量替西罗莫司组(0.1 mg/mL;病变长度0.025~0.050 mg/cm)或高剂量替西罗莫司组(0.4 mg/mL;病灶长度0.10~0.20 mg/cm)。主要终点为6个月时横位血管面积损失百分比(TVAL%);次要终点为6个月时临床相关靶病变失败率(CR-TLF),包括CD-TLR、缺血相关的大截肢、临床相关靶病变闭塞。主要安全终点为30天内无主要不良肢体事件或围手术期死亡(MALE POD)。
研究结果
主要针对符合方案集(PP)组进行统计分析;该组排除了未植入支架的严重解剖或近端全闭塞的受试者,因为这两种情况都可能会导致与目标病变再狭窄无关的早期失败,同时这两种情况也都将在未来的研究登记中被排除。在56例意向治疗(ITT)患者中,随访6个月,8例被排除在PP组。
随访6个月,治疗组在PP和PP-TASC B~D亚组(不包括15例伴有TASC A病变的受试者)中表现出明显的优越性,其中PP-TASC B~D亚组TVAL率为24%,显着低于对照组的46%(图1)。PP和PP-TASC B-D亚组在6个月时TVAL%分别下降13.9%和22.3%。替西罗莫司治疗的患者CR-TLF明显更高,在PP和PP-TASC B~D亚组中,治疗组与对照组在6个月CRTLF的差异分别为27.1%和39.2%(图2)。所有组中30天MALE POD均为100%。

图1. 治疗组和对照组分别在PP-TASC B~D亚组TVAL数据对比
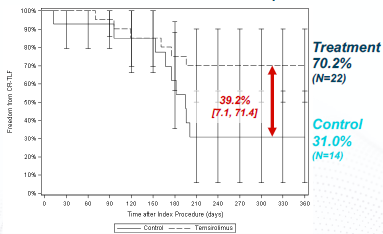
图2. 治疗组和对照组分别在PP-TASC B~D亚组CR-TLF数据对比
总 结
本项研究结果表明,使用Bullfrog MicroInfusion 装置进行替西罗莫司的外膜沉积可在成功进行血管内血运重建后的BTK动脉中改善6个月的血管通畅性。PP和PP-TASC BD亚组的临床疗效指标最有希望,为针对正确患者群体的3期临床试验的资格标准提供指导,以更好地确定该治疗的临床疗效。
王盛,医学博士、主任医师、硕士研究生导师,首都医科大学附属北京安贞医院血管外科。首都医科大学血管外科学系副主任;中国医师协会血管外科分会下肢动脉学组副组长;中国医师协会腔内血管学分委会下肢动脉疾病专家委员会 副主任委员;国际静脉联盟中国静脉学会委员;中国医疗器械协会血管器械分会委员兼副秘书长;中国研究型医院学会血管医学专业委员会委员兼副秘书长;中国医疗保健国际交流促进会血管外科专业委员会常务委员;北京医师协会血管外科专科医师分会常务理事;中华血管外科杂志通讯编委。主要从事血管外科临床和基础研究工作,2011年赴德国莱比锡心脏中心学习血管疾病的腔内治疗,多次到美国、英国、法国等各大血管中心访问交流。2007年获北京市优秀人才基金资助,主持或参与国家自然科学基金、北京市自然科学基金等多项科研课题。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#新思路#
38
#西罗莫司#
35
#TCT#
34
#BTK#
36
#递送系统#
35