3D打印技术辅助湘雅专家完成颅内高难度肿瘤切除手术
2016-04-01 依文 健康界
哑铃状的肿瘤一半在颅内,一半长到颈部,位于颈静脉孔区的肿瘤解剖位置深,周围密布大血管和神经,是神经外科领域中最复杂的高难度手术之一。中南大学湘雅医院神经外科副主任刘庆教授团队成功运用3D打印技术辅助,为一名53岁的女性患者精准微创切除了这一复杂区域的肿瘤,不日即将出院。 全身各部位出状况,原是颅底肿瘤作祟 3年前,廖女士右耳听力开始慢慢下降,随后出现了耳鸣、外耳道流脓等症状,以为是耳朵出了
哑铃状的肿瘤一半在颅内,一半长到颈部,位于颈静脉孔区的肿瘤解剖位置深,周围密布大血管和神经,是神经外科领域中最复杂的高难度手术之一。中南大学湘雅医院神经外科副主任刘庆教授团队成功运用3D打印技术辅助,为一名53岁的女性患者精准微创切除了这一复杂区域的肿瘤,不日即将出院。
全身各部位出状况,原是颅底肿瘤作祟
3年前,廖女士右耳听力开始慢慢下降,随后出现了耳鸣、外耳道流脓等症状,以为是耳朵出了点小问题的她并没有在意。然而,6个月前,她的头部却时不时隐隐作痛,甚至开始恶心呕吐。2个月前更是出现了走路不稳的症状,特别是上下坡时更为明显,声音也开始嘶哑,并且出现了吞咽困难、喝水呛咳等症状。
经检查发现,这些不同部位的奇怪症状,原来都是廖女士颅底的一个肿瘤在作祟。这个肿瘤位于颅底和颈部的交界区“颈静脉孔区”,肿瘤又深藏在密布的大血管和神经中,正是由于压迫了控制听力、吞咽等功能的神经,廖女士才会出现这些症状。

术前
据了解,该部位解剖位置深,无论是从头部还是颈部入路进行手术,显露都非常困难,很难一次性完全切除。此外,这一区域解剖结构十分复杂,骨质非常不规则。这一近于“未知”而复杂的区域,对于手术来说是一大挑战。
3D技术助力精准直达肿瘤
如何寻找最佳治疗方法,这个艰难的问题同时摆在神经外科和耳鼻咽喉头颈外科专家面前。
对于神经外科专家来说,切除这一交界区的复杂肿瘤,传统开颅手术从颅内往颅底切除肿瘤,“哑铃”在颅内的一端肿瘤能够切除,但颈部的另一端“哑铃”就无法切除干净;而耳鼻咽喉头颈外科专家从颞下窝入手,从外往颅底切,能够解决颈部的“哑铃”,却无法将颅内的一端切除干净;即使与口腔科协作,从面部把下颌骨截断,肿瘤仍然显露困难,无法完全切除。
“传统的方法不仅需要在耳后和脖子上做一个很大的切口,大概半个脑袋都需要显露出来。更为麻烦的是,肿瘤很难切除干净。”据湘雅医院神经外科副主任刘庆教授介绍,其团队在袁贤瑞教授的带领下,就如何选择最适合的入路,以最小的创伤最干净地切除颈静脉孔区肿瘤进行了10余年的潜心研究。专家们发现,“开门见山”是最适合的方法,直奔交界区将周围的骨头切除,把肿瘤边界暴露。
那么,为了尽可能地减少患者的创伤,切除多少骨头合适呢?刘庆教授团队决定借力最新的3D打印技术,通过高清晰的影像,重建患者脑部3D模型,在模型上反复模拟制定最合适的手术方案,有选择性地切除最少的骨头,能够精准直达肿瘤所在的位置。
术前“预演”辅助避开大血管并保护神经功能
切除肿瘤的最终目的是提高患者的生活质量,尽最大可能保留和恢复正常的神经功能。然而,这个位置的肿瘤深藏在密布的大血管和神经之中,不仅有颈内动脉、颈内静脉、椎动脉等脑部重要血管,更有后组颅神经区,包括舌咽神经、迷走神经、副神经、舌下神经等。
如何不损伤这些重要的血管和神经呢?3D打印的模型可以还原肿瘤在颅内的真实情况,清晰地显示肿瘤与这些血管和神经的关系,专家们术前就可以制定和“预演”最合适的手术方案,精准地避开这些重要的血管和神经。


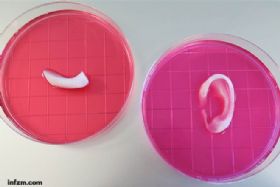
3D打印的模型
3月16日,刘庆教授和袁健博士团队,成功地为廖女士进行了手术。专家们按照在3D模型上预演的手术方案,有选择性地磨掉了交界区的一部分骨头,将肿瘤边界暴露出来。从位于颈部的肿瘤根部往外开始切除一端的肿瘤,再往里“掏”出“哑铃”肿瘤在颅底的一端,完整地切除了直径4厘米的肿瘤。
“整个手术几乎都是在硬膜外进行操作,对于硬膜内的神经、血管和脑组织都有一定的保护作用,基本上没有牵引脑组织,保护了正常的神经功能。”刘庆教授介绍,这都得益于3D打印技术的辅助。

术后
传统手术因无法如此精确地保护神经和血管,患者术后需要用胃管鼻饲1-2个星期,以防误吸入气管危及生命。而廖女士术后可立即正常进食,听力渐渐恢复了,声音嘶哑的状况也有所好转,正在逐渐恢复正常的神经功能,不日即可出院。
3D打印“克隆”颅内肿瘤 高难手术不再凭空想象
名词解释---E-3D数字化医疗三维设计系统
采用最新的数字化技术,结合医学、计算机、虚拟现实、图形学等多学科交叉研究开发,将多种仪器检查的图像数据相互融合,实现多模态影像学数据彼此之间或整体之间的无缝对接,根据需要显示出病灶或周围组织和器官,象“堆积木”一样动态地任意增减所需要显示的组织、器官,并使之转化为可视的三维图像。
湘雅医院研发E-3D数字化医疗三维设计系统为一脑瘤患者切除肿瘤
通过3D打印技术,能1:1打印人体颅内肿瘤模型,甚至肿瘤与血管之间的复杂连接、肿瘤表面的凹凸不平等,都能清晰地“克隆”出来。昨日,中南大学湘雅医院对外宣布,该院利用这一技术精准切除一颗复杂颅内肿瘤,根据文献检索发现,此举在全球尚未见报道。
3D打印“克隆”颅内复杂肿瘤
患者张某因头痛、恶心、呕吐、性格改变、记忆力下降持续3年,近一个月症状加重来到湘雅医院求医,被确诊为鞍结节脑膜瘤。患者入院时,颅高压症状十分明显,不尽快手术的话随时可能有生命危险。然而,该患者颅底肿瘤位置深,肿瘤与颈内动脉、视神经、垂体柄等周边重要结构关系复杂,手术难度十分大。
为了提高手术的精准度,湘雅医院专家团队通过自主研发的E-3D数字化医疗三维设计系统,将患者CT和MRI扫描获得的影像学数据融合,并作进一步精细化处理,获取精确化空间数据,转化重建为三维模型,将颅底复杂肿瘤和毗邻血管及神经等组织区分,结合3D打印技术,成功将该患者的颅底肿瘤及周围组织等比例地精准打印出来。
“这个打印模型完全可以称得上是患者颅内肿瘤的‘克隆产品’。”湘雅医院肿瘤科黄俊辉教授介绍,模型完全按照肿瘤的实际比例打印而成,材质是不同的高科技分子材料,精确地复制了具有复杂形态、不同质地和密度的人体肿瘤解剖结构。
用3D技术打印出的肿瘤模型边界清晰,甚至患者的头颅骨、肿瘤相连及周围的血管都打印出来了。黄俊辉教授说:“肿瘤在颅底的什么位置,周围有什么血管,一目了然。”
高难度手术不再“凭空想象”
该团队核心成员、湘雅医院神经外科李学军副教授介绍,颅底肿瘤是外科手术中难度最高的一项手术,传统手术主要依据患者的CT和MRI(核磁共振)图像,但二者存在有平面化的局限性,因此需要医生有一个立体空间的想象力,才能为接下来的手术做好铺垫,“即使是具有丰富临床经验的医生,也很难做到在手术中百分之百的精准,因为有些肿瘤周围组织结构复杂,手术边界较为模糊,手术容易留下死角。”
“3D打印的肿瘤原型给了医生充分的手术设计辅助,主要是优化手术设计。”李学军介绍,3D打印技术能让医生在手术前充分了解脑内肿瘤的部位、形状、大小及与周围组织的毗邻关系,确定手术进入路线、切除范围、术中注意事项等,能在完整切除肿瘤的同时最大限度地保护肿瘤周围正常组织,降低了并发症和后遗症的发生率。与传统的手术相比,应用3D打印技术的手术更具精准度和前瞻性。
1月2日,以李学军副教授为首的专家组,成功为患者实施了肿瘤切除手术。患者术后恢复良好,头痛、恶心、呕吐、记忆力下降等症状得到明显改善,且没有出现神经功能障碍。
据中南大学计算机视觉与虚拟现实技术研究所副所长廖胜辉副教授介绍,除了本次复杂颅内肿瘤模型之外,他们还在对肝脏、肾脏疾病的3D打印技术加紧研究,未来有望看到人体各种复杂器官疾病的3D打印模型。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#肿瘤切除#
42
#3D打印技术#
35
3D是趋势
134
模型重建,好想法
173
3D打印让治疗可视化,精准化!
117
#3D#
32
#切除手术#
33
#湘雅#
33