Eur Heart J:“抑郁和冠心病”声明:建议冠心病患者筛查抑郁,怀疑者应转专科治疗
2019-02-26 卢芳 中国循环杂志
近日,欧洲心脏病学会(ESC)发布关于抑郁和冠心病立场文件,指出15~30%的冠心病患者伴有抑郁,比普通人群高2~3倍。女性约为男性2倍,尤其是年轻女士急性心肌梗死患者。
近日,欧洲心脏病学会(ESC)发布关于抑郁和冠心病立场文件,指出15~30%的冠心病患者伴有抑郁,比普通人群高2~3倍。女性约为男性2倍,尤其是年轻女士急性心肌梗死患者。
而且冠心病和抑郁存在恶性循环,冠心病患者中抑郁较常见,而抑郁者预后较差。
冠心病合并抑郁者常发生的气短和(或)胸痛与冠心病严重程度无关,比其他传统危险因素预测性更强。
这可能与抑郁和胸痛有共同的神经激素途径和遗传背景有关。
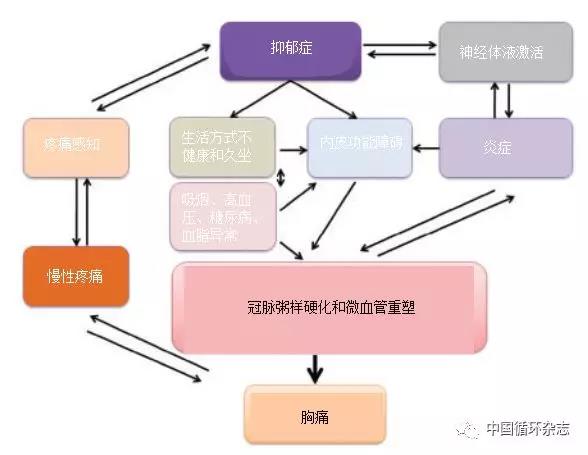
图1 冠心病患者中抑郁和胸痛的关系
冠心病合并抑郁预后较差的潜在机制是复杂和多因素的,其中植物神经功能紊乱、炎症、内皮功能紊乱、血小板活化和血栓形成、生活行为和心脏代谢危险因素等都交织其中。
文件强调,识别和纠正抑郁是提高冠心病患者生存质量的可改善因素,临床医生应加强认识。
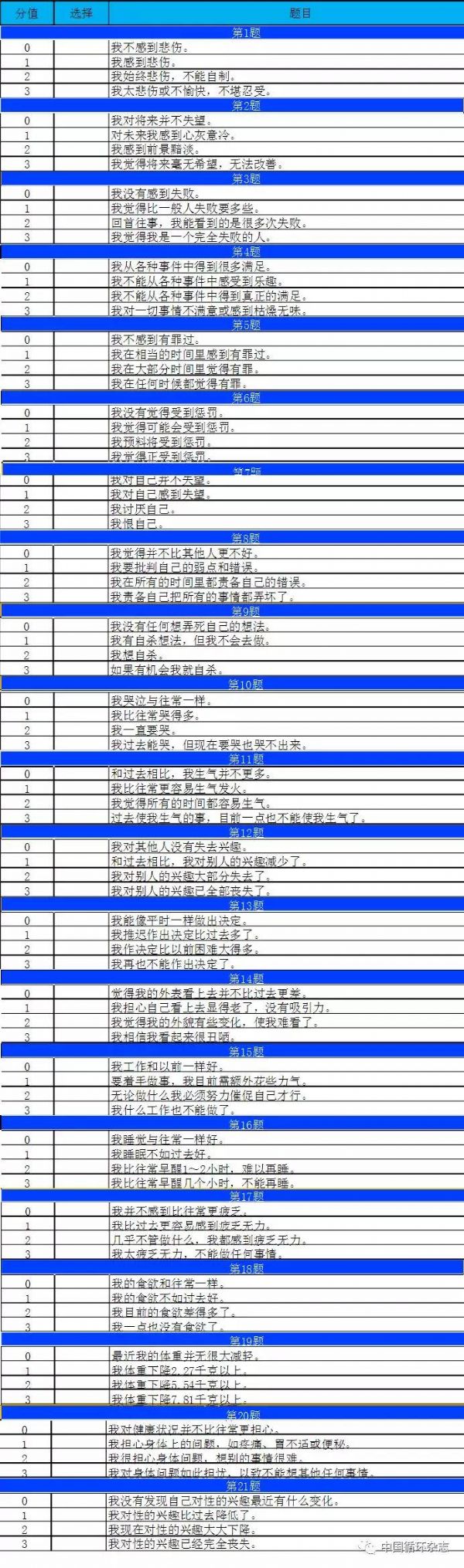
文件指出,对于繁忙的心脏科,贝克抑郁自评量表较为实用,有助于可靠筛查抑郁状况。
在治疗方面,药物治疗、各种形式心理治疗、运动和压力管理等均可选择。
文件指出,尽管治疗抑郁能改善心血管疾病预后尚未证实,但对于严重抑郁的冠心病患者,处理抑郁有助于促进患者健康和提高生活质量。
其中,三环类抗抑郁药物在冠心病合并抑郁患者中应避免使用。
总之,文件推荐:
1. 临床医生应该明了冠心病患者中抑郁的较高共患情况,争取对冠心病患者中筛查抑郁。
2. 对于怀疑抑郁的冠心病患者,应该移交到专科医生诊疗。
3.可考虑运动和心理治疗等非药物治疗。
4. 对于冠心病合并抑郁的患者,多学科治疗必不可少。
附贝克抑郁量表(Beck Depression Inventory):
根据下表自我评估,共21题:
总分10分:很健康、无抑郁;
总分10分~15分:有轻度情绪不良,要注意调节;
总分大于15分者:已有抑郁,需要去看心理医生;
总分大于25分:抑郁严重,必须看心理医生。
原始出处:Viola Vaccarino Lina Badimon J Douglas Bremner, et al. Depression and coronary heart disease: 2018 ESC position paper of the working group of coronary pathophysiology and microcirculation developed under the auspices of the ESC Committee for Practice Guidelines. Eur Heart J, 28 January 2019
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









真的挺好
126
#ART#
42
#冠心病患者#
40
#HEART#
35
#专科#
37
学习学习学习
72
学习了很有用不错
77