Neurosurg Focus:三柱截骨术并发症率与脊柱融合相当
2014-07-09 phdyhm 丁香园
重度脊柱畸形往往被认为是多平面复杂性脊柱畸形,伴有侧凸、后凸及前凸中的一种或多种,其椎体间柔韧性明显下降,脊柱严重不平衡,只有手术才能较好的恢复生理上整体性和局部性的平衡。在脊柱畸形的手术治疗中,脊柱融合术是应用最为广泛的一种。在脊柱融合术应用的半个多世纪里,“融合”早已成为脊柱畸形治疗的“金标准”。 随着现代脊柱外科矫形技术的不断发展,对重度脊柱畸形,尤其是重度僵硬性脊柱畸形,单纯脊柱融合
重度脊柱畸形往往被认为是多平面复杂性脊柱畸形,伴有侧凸、后凸及前凸中的一种或多种,其椎体间柔韧性明显下降,脊柱严重不平衡,只有手术才能较好的恢复生理上整体性和局部性的平衡。在脊柱畸形的手术治疗中,脊柱融合术是应用最为广泛的一种。在脊柱融合术应用的半个多世纪里,“融合”早已成为脊柱畸形治疗的“金标准”。
随着现代脊柱外科矫形技术的不断发展,对重度脊柱畸形,尤其是重度僵硬性脊柱畸形,单纯脊柱融合术后畸形的矫正效果不佳,因而目前矫正手术已从传统的后路单纯多棒撑开内固定或前路松解后路内固定等逐步向截骨矫形术转变。截骨术可以明显提高重度僵硬性脊柱侧凸的矫正效果,是脊柱侧凸矫形方法的新发展。
三柱截骨术在后柱截骨术的基础上发展而来,截骨涉及整个脊柱的前、中、后柱,可使脊柱重排,矫形效果更好。三柱截骨术主要包括经椎弓根楔形截骨(PSO),全脊椎切除术(VCR),以及在VCR基础上发展而来的脊柱去松质骨截骨及多节段椎体截骨。
三柱截骨术是治疗重度僵硬性脊柱侧凸的有效方法之一,但也存在风险大、 技术难度高等缺点,特别是神经系统损伤等并发症发生率较高。为了进一步比较三柱截骨术与后路脊柱融合术后并发症的发生率以及分析并发症的危险因素,美国学者Kelly等进行了一项多中心队列研究,该研究结果已在近期的Neurosurg Focus杂志上发表。
在该研究中,研究者于2009年1月1日至2011年1月1日期间在美国5个医学中心招募207例成人脊柱畸形患者作为研究队列,并将该前瞻性研究队列命名为Scoli-RISK-1。在Scoli-RISK-1研究队列中,75例患者行后路脊柱融合,132例行三柱截骨术。分别比较两组患者的人口统计学数据、手术数据、以及围手术期并发症,并将各种患者数据与并发症发生率进行回归性分析,以确定并发症的相关危险因素。

表2. 术前人口统计学数据

三柱截骨术组患者术前的矢状位移位为11.7cm,后路脊柱融合组患者的术前移位为5.4cm,两组之间的差异显著;但两组患者的术前矢状位Cobb角却无显著性差异,分别为45.8°与57.7°。
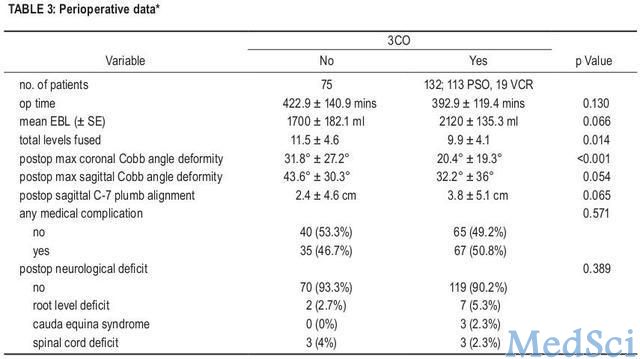
在手术数据的比较中,两组患者的手术时间相近,分别为393与423分钟。三柱截骨术组患者的估计失血量平均为2120ml,高于后路脊柱融合组患者的1700ml失血量,但两组之间的差异仍不显著。
在并发症方面,两组患者的神经功能缺失以及其他围手术期并发症发生率相当,三柱截骨术组与后路脊柱融合组患者的神经功能缺失并发症发生率分别为9.9%与6.7%,而其它围手术期并发症发生率分别为50.8%与46.7%。
在三柱截骨术组的患者中,行VCR手术治疗的患者的并发症发生率为73.7%,显著高于行PSO手术患者46.9%的并发症发生率;但VCR与PSO患者的神经功能缺失并发症发生率却并无显著性差异,分别为15.8%与8.8%。对人口统计学数据、手术数据与并发症发生率进行回归性分析,结果发现这些数据均不是并发症发生率的显著相关危险因素。
表3. 围手术期数据
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#截骨术#
44
#并发#
37
#ROS#
38
#融合#
26