JCI:重大发现!提出甲状腺瘤产生新理论
2016-08-16 佚名 生物谷
自主功能性甲状腺腺瘤(autonomous thyroid adenoma, ATA)是最为常见的甲状腺良性肿瘤。两种基因发生的突变导致大约70%的ATA病例。如今,在一项新的研究中,来自德国维尔茨堡大学的研究人员发现另外一种关键性的触发因子。相关研究结果于2016年8月8日发表在Journal of Clinical Investigation期刊上,论文标题为“Recurrent EZ
自主功能性甲状腺腺瘤(autonomous thyroid adenoma, ATA)是最为常见的甲状腺良性肿瘤。两种基因发生的突变导致大约70%的ATA病例。如今,在一项新的研究中,来自德国维尔茨堡大学的研究人员发现另外一种关键性的触发因子。相关研究结果于2016年8月8日发表在Journal of Clinical Investigation期刊上,论文标题为“Recurrent EZH1 mutations are a second hit in autonomous thyroid adenomas”。
甲状腺激素参与控制人体的很多功能:它们影响糖、脂质和蛋白代谢,调节体温、心率、血液循环和更多的功能。在儿童中,它们也控制大脑和神经发育以及骨生长。这也难怪甲状腺机能亢进对受影响的病人产生几种有害的影响。典型特征包括持续的坐立不安、易怒、令人费解的体重减少、出汗过多和脉压增加。甲状腺机能亢进在未加治疗时会产生严重的后果,包括最为重要地,更高的心血管疾病死亡率。
寻找作为病因的突变
在许多情形下,这种机能亢进是由甲状腺瘤导致的,其中大多数甲状腺瘤是良性的。在甲状腺瘤当中,所谓的ATA占绝大多数。一般而言,它的起源得到很好理解:“我们知道某些基因中的特定突变导致大约70%的ATA”,论文第一作者、维尔茨堡大学药理学与毒理学学院研究员Davide Calebiro博士说。
具体而言,人们在高达70%的ATA中发现TSHR基因(编码促甲状腺激素受体)的激活突变。此外,一小部分ATA在GNAS基因(编码Gs蛋白α亚基)上发生激活突变。
然而,在此之前,人们并不清楚这些突变独自是否足以促进甲状腺细胞增加和产生过量的激素,或者说,是否还必须存在其他的因子。此外,人们也不清楚哪些因子参与剩下30%的ATA病例产生。
发表在期刊上
在寻找ATA的其他病因中,由Davide Calebiro、来自意大利米兰大学的Luca Persani和来自加拿大卡尔加里大学的Ralf Paschke领导的一个国际团队如今取得成功。
Calebiro描述了他们的方法,“就我们的研究而言,我们利用全外显子测序研究了19种ATA病例。”这种技术并不研究细胞的全基因组,而是研究基因的外显子,即真正地翻译为蛋白的DNA片段。通常而言,这些外显子(外显子组)占总DNA的1~2%。Calebiro进一步解释道,“我们能够证实在这些ATA中,有相当数量的ATA在一个参与控制细胞增殖和分化的基因中发生突变。”
基因突变导致细胞增殖增加
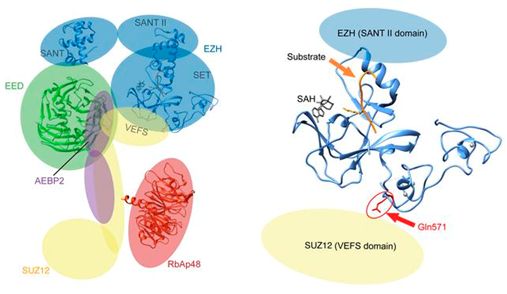
这个基因的科学名字就是EZH1(Enhancer of Zeste Homolog 1)。EZH1基因突变与其他已知的突变协同发挥作用,从而导致ATA产生。再者,功能性研究证实EZH1基因突变让导致甲状腺细胞增殖的信号通路发生变化。
Calebiro总结道,“我们证实EZH1基因发生的一种热点突变是ATA的第二种最为常见的基因缺陷。”在他看来,EZH1基因突变与之前已知的基因中发生的那些突变经常关联在一起,这就表明存在一种“两次打击模型”。相应地,第一种基因突变增加形成ATA的易感性,而第二种基因突变触发这种疾病过程。
原始出处
Davide Calebiro, Elisa S. Grassi,3 Markus Eszlinger,4,5 Cristina L. Ronchi,6 Amod Godbole,1,2 Kerstin Bathon,1,2 Fabiana Guizzardi,3 Tiziana de Filippis,3 Knut Krohn,7 Holger Jaeschke,5 Thomas Schwarzmayr,8,9 Rifat Bircan,10 Hulya Iliksu Gozu,11 Seda Sancak,12 Marek Niedziela,13 Tim M. Strom,8,9 Martin Fassnacht,6,14 Luca Persani,3,15 and Ralf Paschke.Recurrent EZH1 mutations are a second hit in autonomous thyroid adenomas.JCI.2016
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








学习了谢谢作者分享!
59
#甲状腺瘤#
33
#JCI#
0
#重大发现#
29
值得学习
44
学习了,希望多点研究,特别是基层研究
50
继续学习
0
继续关注
55
好好学习一下
25