Lancet Oncol:FOLFOX方案加西妥昔单抗用于结直肠癌维持治疗方案(COIN-B研究)
2014-04-28 MedSci MedSci原创
晚期结直肠癌可使用细胞毒药物和靶向药物的联合治疗,一直以来临床上的治疗策略都是主张连续化疗直至患者不能耐受。但随着新药的应用,晚期结直肠癌患者的生存期延长,化疗毒性作用的累积,使患者很难长期承受相同强度的治疗。如何才能将细胞毒药物治疗时间降至最低以及分子靶向疗法是否能进一步改善等尚不清楚。为此,一项研究旨在确定西妥昔单抗怎样才能安全有效的加入到间歇化疗中。研究结果本月发表在线于《柳叶刀 肿瘤学》杂
晚期结直肠癌可使用细胞毒药物和靶向药物的联合治疗,一直以来临床上的治疗策略都是主张连续化疗直至患者不能耐受。但随着新药的应用,晚期结直肠癌患者的生存期延长,化疗毒性作用的累积,使患者很难长期承受相同强度的治疗。如何才能将细胞毒药物治疗时间降至最低以及分子靶向疗法是否能进一步改善等尚不清楚。
为此,一项研究旨在确定西妥昔单抗怎样才能安全有效的加入到间歇化疗中。研究结果本月发表在线于《柳叶刀 肿瘤学》杂志
COIN-B是一项开放标签,多中心,随机,探索性2期试验,该试验在英国的30家医院及塞浦路斯的1家医院进行。参加试验的患者为既往未接受过解救化疗治疗的转移性晚期大肠癌患者。患者按1:1比例进行随机,分别接受间歇化疗+西妥昔单抗或间歇化疗加持续西妥昔单抗治疗。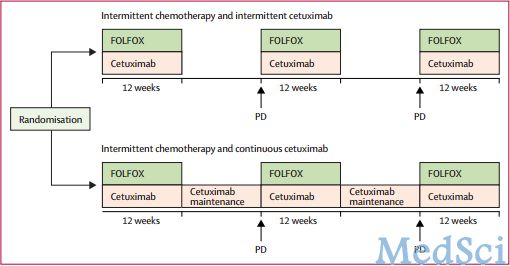
化疗为FOLFOX方案(亚叶酸联合奥沙利铂,推注和输注氟尿嘧啶)。两组患者接受FOLFOX方案以及西妥昔单抗周疗治疗12周,然后按计划中断治疗(间歇西妥昔单抗治疗组患者),或继续西妥昔单抗周疗维持治疗(连续西妥昔单抗治疗组患者)。RECIST(实体瘤疗效评估标准)进展后,再次给予FOLFOX联合西妥昔单抗治疗12周,之后进一步中断或维持西妥昔单抗治疗。
主要研究终点为10个月时的无失败生存率。主要分析对象包括完成了12周治疗但没有进展,死亡或离开试验的患者。并回顾性的检测了BRAF和NRAS状态。
研究登记了401例患者,226人纳入研究。169例为KRAS野生型,78例(46%)进行间歇西妥昔单抗治疗,91例(54%)进行连续西妥昔单抗治疗。初步分析中包括64例患者间歇西妥昔单抗治疗患者和66例连续西妥昔单抗治疗患者。
两组患者无失败生存率的km曲线
间歇组10个月无失败生存率为50%(95%CI 下限为39),连续组为52%(95%CI 下限为41);中位无进展生存期分别为12.2个月(95%CI 8.8-15.6)和14.3个月(95%CI 10.7-20.4)。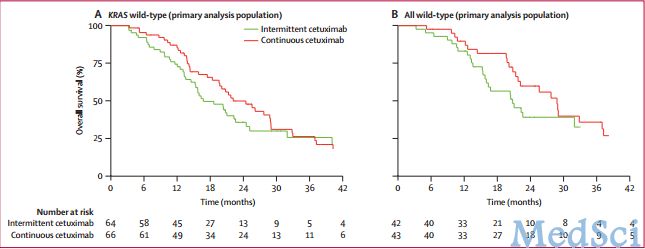
两组患者总生存的km曲线
此外,持续治疗组具有更长的无化疗间歇期(CFI,5.5个月对3.7个月)、首次化疗后间隔期的中位PFS期(5.8个月对3.1个月)和OS期(22.2个月对16.8个月)。
最常见的3-4级不良反应为皮疹(21/77[27%]:20/92[22%] ),中性粒细胞减少(22[29%]:30[33%]),腹泻(14[18%]:23[25%]),以及嗜睡(20[26%]:19[21%])。
西妥昔单抗持续应用作为化疗间歇期的维持治疗是安全的。在最初治疗的6个月中,采用较少的细胞毒药物化疗以及生物靶向药物单药维持治疗这种治疗策略是具有应用前景的,但该结果还需要在Ⅲ期研究中进行验证。
原始出处:
Wasan
H, Meade AM, Adams R, Wilson R, Pugh C, Fisher D, Sydes B, Madi A,
Sizer B, Lowdell C, Middleton G, Butler R, Kaplan R, Maughan T; on
behalf of the COIN-B investigators.Intermittent chemotherapy plus either intermittent or continuous cetuximab for first-line treatment of patients with KRAS wild-type advanced colorectal cancer (COIN-B): a randomised phase 2 trial.Lancet Oncol. 2014 Apr 2. pii: S1470-2045(14)70106-8.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Lancet#
37
#治疗方案#
29
#Oncol#
39
#西妥昔#
45
#结直肠#
31
#FOLFOX#
36