Nature Medicine:足细胞suPAR、APOL1变异和αvβ3整合素三复合体对介导了慢性肾脏病!
2017-06-27 xing.T MedSci原创
在小鼠中,研究人员发现APOL1基因的G1或G2变异亚型增加了αvβ3整合素的活化,并且导致了suPAR依赖性的尿蛋白。循环因子suPAR和APOL1基因G1或G2变异亚型对αvβ3整合素活化的协同作用是一种导致慢性肾脏病的发病机制。
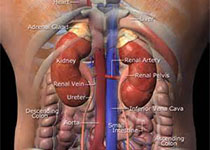
可溶性尿激酶型纤溶酶原激活物受体(suPAR)可以独立预测慢性肾脏疾病(CKD)的疾病发生和病情进展。在新近的非洲血统的个体中,载脂蛋白L1(APOL1)基因的变异亚型G1和G2,而不是参考的等位基因(G0),与慢性肾脏病的风险增加存在相关性。
近日,权威杂志Nature Medicine上发表了一篇研究文章,在这个研究中,研究人员通过两个大型的、无任何相关性的队列展示了肾功能的下降与APOL1危险变异相关,并且这种相关性是依赖于血浆中的suPAR水平:APOL1相关的风险在低suPAR水平的患者中显著减弱,而在那些suPAR水平较强的患者中明显增强。在机制上,研究人员通过表面等离子体共振检测发现suPAR、APOL1和αvβ3整合素之间存在高亲和力的相互作用,而APOL基因的G1和G2变异亚型展示出了比APOL1基因G0更高的suPAR激活的αvβ3整合素的亲和力。
在小鼠中,研究人员发现APOL1基因的G1或G2变异亚型增加了αvβ3整合素的活化,并且导致了suPAR依赖性的尿蛋白。循环因子suPAR和APOL1基因G1或G2变异亚型对αvβ3整合素活化的协同作用是一种导致慢性肾脏病的发病机制。
原始出处:
Salim S Hayek,et al. A tripartite complex of suPAR, APOL1 risk variants and αvβ3 integrin on podocytes mediates chronic kidney disease.Nature medicine, 2017. https://www.nature.com/nm/journal/vaop/ncurrent/full/nm.4362.html
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#复合体#
31
#DIC#
36
#CIN#
27
#Nat#
29
#uPAR#
46
#变异#
39
#整合素#
29
#Medicine#
22
#Med#
24
#慢性肾脏#
25