J Cell Biochem:警惕老年人补钙的心血管并发症
2015-02-09 梁怀彬 译 MedSci原创
长期以来人们众所周知:补充钙剂有可能增加肾功能不全病人发生心血管疾病的风险。最近“奥克兰钙实验”的研究学学者表明,这些心血管事件风险也可能发生在希望通过使用钙剂达到预防骨质疏松症目的的老年人身上。研究者后续的Meta-分析亦证实,老人补充钙剂,无论与此同时补充或者不补充维生素D,都对于心血管系统有着一定程度不利的影响——增加心肌梗死和脑卒中的发生风险。 Kaplan–Meier生存曲线(心梗及中风
长期以来人们众所周知:补充钙剂有可能增加肾功能不全病人发生心血管疾病的风险。最近“奥克兰钙实验”的研究学学者表明,这些心血管事件风险也可能发生在希望通过使用钙剂达到预防骨质疏松症目的的老年人身上。研究者后续的Meta-分析亦证实,老人补充钙剂,无论与此同时补充或者不补充维生素D,都对于心血管系统有着一定程度不利的影响——增加心肌梗死和脑卒中的发生风险。
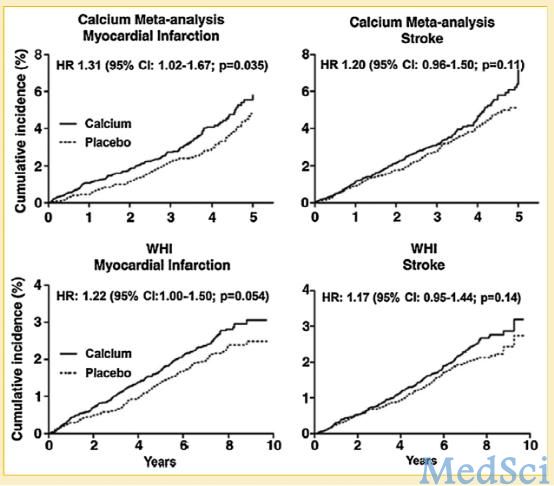
Kaplan–Meier生存曲线(心梗及中风发生率) 上部分:Meta分析结果(n=8151)
下部分:WHI妇女补钙倡导中定量定时补钙人群结果(n=16718)
一些团队重新对现已发表的文章统计分析显示,补钙存在诱发心肌梗死的副作用。不同的研究这种影响差别不一致,一些Meta-分析由于研究质量限制,亦得出没有显著统计学差异的结论。研究者说,之所以现在关于补钙能否诱发心梗等心血管事件存在争议以及不同Meta分析结果存在矛盾,取决于研究者是否将下列两个特别的分组也纳入了研究,一是在“世界妇女健康倡议”(Women`s Health Initiative,WHI)号召下,进入研究前生活中就一直随时服用钙剂的人群,她们的补钙个性化且随意化;二是实验人群的纳入是来自于两个基线心血管发病风险就不相同的两个个体人群。
研究者进一步指出,单纯只补充维生素D并不增加心血管事件发病风险。所以单独使用钙剂抑或着钙剂、维生素D联合使用,两者之间心血管副作用没有差异,而有的研究指出存在差异很可能是由于纳入研究的样本存在偏差所致。
钙剂之于心血管系统的不利影响的具体机制是现在还不是很明确,但很有可能是通过钙的摄取增加使血清钙增加并因此影响血管功能和凝血功能这一机制来介导的。因此研究者在结论里写道,老年人补钙所诱发的心血管事件风险可能大于预防骨折发生的微小利益,所以心血管疾病风险高的老年人补钙须慎重。
原始出处:
Reid IR, Bristow SM, Bolland MJ.Cardiovascular complications of calcium supplements.
J Cell Biochem. 2015 Apr;116(4):494-501. doi: 10.1002/jcb.25028.
本文是MedSci原创编译整理,转载需要事先获得授权!转载需要附来源及MedSci 原始链接。谢谢!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











没有科学依据
63
#CEL#
29
#Bio#
40
#并发#
37
#Cell#
0
重视
85
患OS这个疾病的高风险人群提供干预措施以避免不良预后和机械治疗措施
104
应该重视下!学习了!
139
不错,不错,学习!
93
学习了很好的资讯
68