Clin Infect Dis.:哪些类型癌症患者活动性结核进展风险**?
2017-04-02 贾朝娟 环球医学
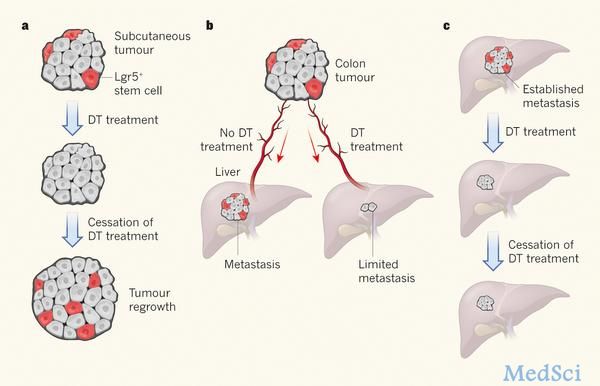
癌症可增加活动性结核进展的风险,但哪些类型癌症的风险最大呢?2017年3月1日发表在《Clin Infect Dis》的一项研究显示,血液学、头颈部和肺癌患者活动性结核进展率比其他癌症患者高9倍。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#活动性#
27
#Dis#
28
#结核#
28
#癌症患者#
36
学习了,多谢分享
52
可能与该肿瘤免疫抑制能力更强有关!反之这些肿瘤免疫治疗效果可能会更好!
53
学习了谢谢分享
56
学习了谢谢分享
56
学习了很有用
48