NEJM:Tabrecta治疗METex14跳跃的非小细胞肺癌,关键研究取得积极结果
2020-09-03 Allan MedSci原创
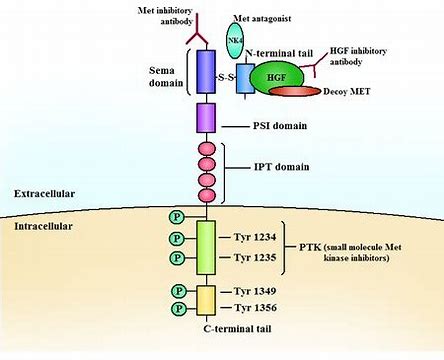
MET是由MET基因编码的受体酪氨酸激酶,通常在细胞信号传导、增殖和存活中起重要作用。
近日,在《新英格兰医学杂志》(NEJM)上发表的关键性GEOMETRY mono-1 II期研究的数据显示,使用Tabrecta™(capmatinib)治疗MET外显子14(METex14)跳跃非小细胞肺癌的总缓解率(ORR)和反应持续时间(DOR)取得积极结果。
MET是由MET基因编码的受体酪氨酸激酶,通常在细胞信号传导、增殖和存活中起重要作用。许多癌症与MET受体途径的异常信号传导有关,这是由多种机制引起的,包括点突变、插入/缺失导致外显子14的跳跃。
诺华肿瘤学开发主管Jeff Legos说:“今天发表的数据不仅证实了我们之前在非小细胞肺癌中使用Tabrecta治疗所获得的积极结果,而且还强调了对患者肿瘤进行早期和广泛分子检测的价值,以指导治疗方案。我们知道患有这种侵袭性肺癌的患者预后较差,他们往往年龄较大。我们致力于与全球卫生当局合作,尽快将Tabrecta带给患者”。
独立放射学委员会(BIRC)对Tabrecta治疗MET外显子14跳跃患者(n = 97)进行了ORR分析,结果显示,初治患者(n = 28)的ORR率为68%(95%CI 48-84);先前接受过治疗的患者(n = 69)的ORR率为41%(95%CI 29-53)。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#MET#
38
#非小细胞#
0
#Tabrecta#
36
#CTA#
46
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
56
很好
82