J Clin Oncol:第一个多队列篮子试验——MyPathway初步研究结果发布
2018-01-15 肿瘤资讯编辑部 肿瘤资讯
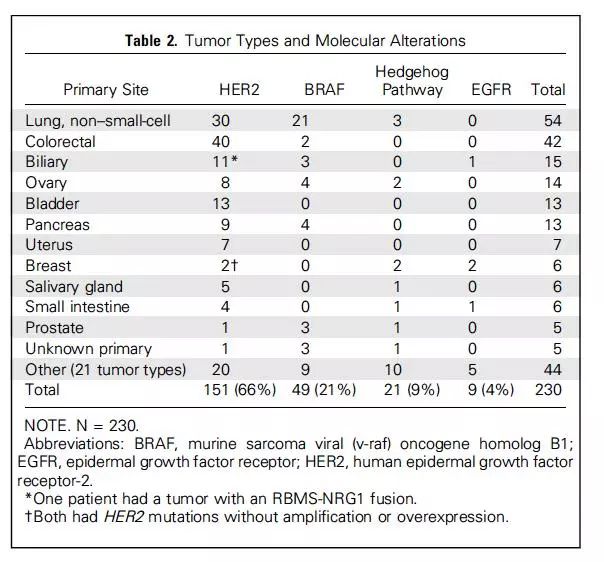
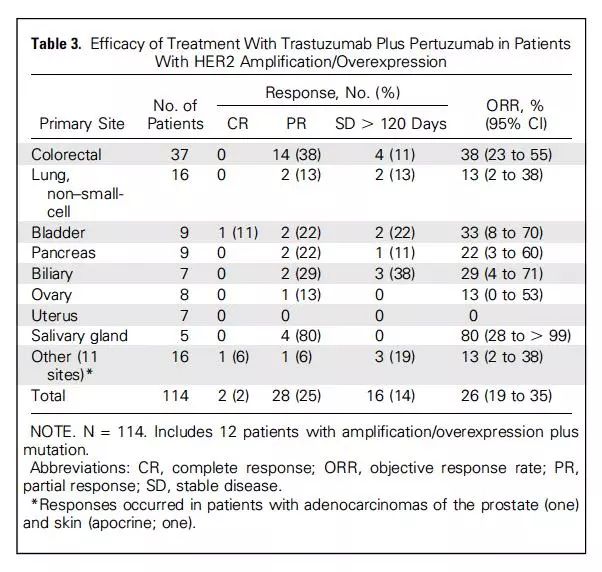
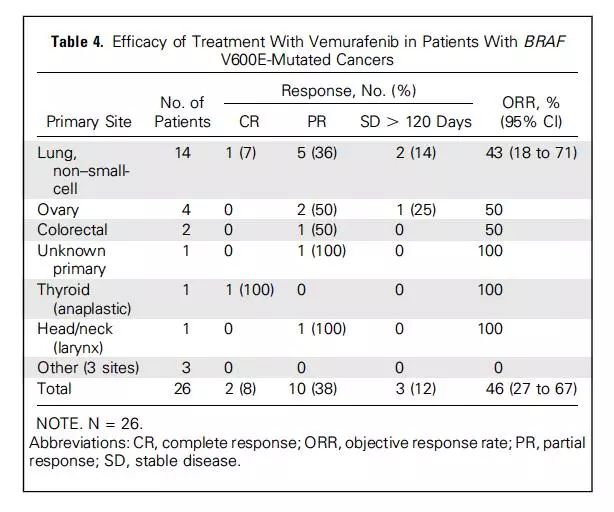
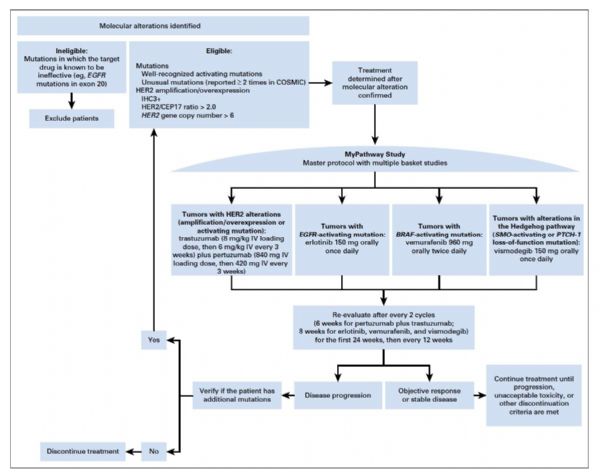
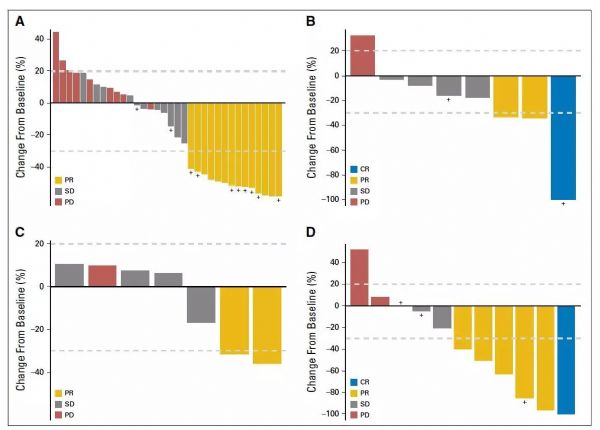
随着二代测序的应用,越来越多低频突变被发现。因基因变异频率较低,如果采用传统的临床试验方式进行研究,很难达到统计学要求的样本量,为此,创新性的临床试验诞生——篮子试验和雨伞试验。其中,MyPathway研究就是一个经典的多队列篮子试验。近日,《JCO》杂志发布了MyPathway研究的初步结果。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#研究结果#
31
#Oncol#
32
#pathway#
37
学习了谢谢分享!!
60
好资料学习了!
50
学习了谢谢分享!!
50
好资料学习了!
64