病例分享:发热咳嗽治不好,元凶竟是脓肿灶
2017-09-19 张尧、金文婷 SIFIC感染官微
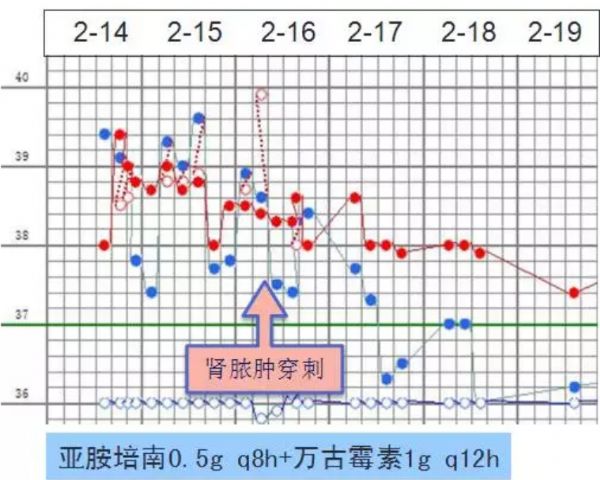
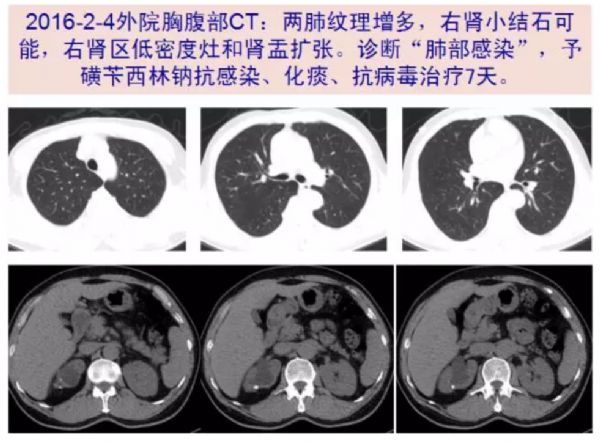
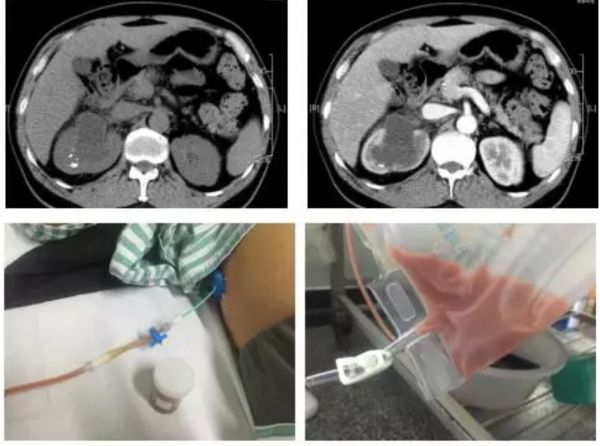
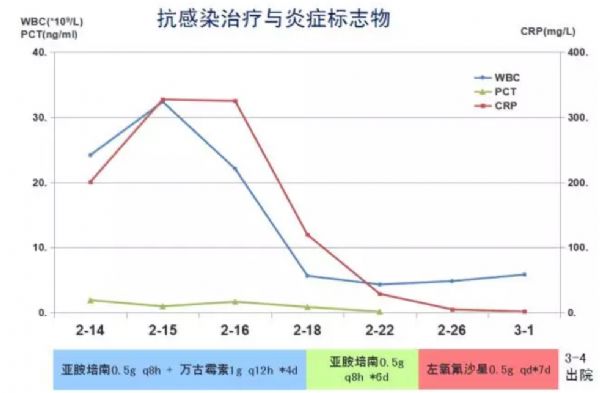
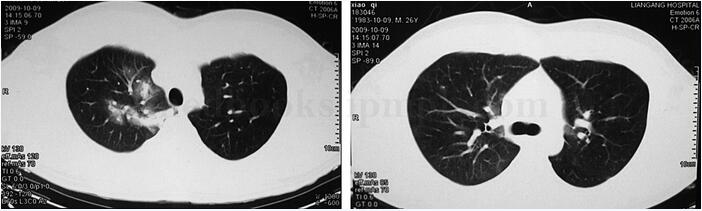
呼吸道感染是引起发热最常见的类型,但临床上不能只关注呼吸道症状而忽略其他部位感染的表现。本例发病初期即有尿路刺激征和尿常规异常,甚至CT提示肾脏低密度阴影,然仍被临床医生明显忽视了,当作肺部感染予以治疗。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#脓肿灶#
20
#脓肿#
22
学习了
55
引流比抗生素作用更强大?
63
学习了受益匪浅
60