确诊左心房罕见恶性肿瘤 超声心动图捕获线索
2017-09-18 朱天刚 超声心动图与临床决策:疑难病例解析
中年女性,因反复咳嗽2个月入院,超声心动图提示左心房黏液瘤、少量心包积液,行手术切除肿物,结合病理报告最终确诊为左心房内膜肉瘤侵及肺静脉。由此罕见病例引发深入思考:内膜肉瘤的临床特征是什么?怎样鉴别诊断心脏内异常回声超声心动图?
中年女性,因反复咳嗽2个月入院,超声心动图提示左心房黏液瘤、少量心包积液,行手术切除肿物,结合病理报告最终确诊为左心房内膜肉瘤侵及肺静脉。由此罕见病例引发深入思考:内膜肉瘤的临床特征是什么?怎样鉴别诊断心脏内异常回声超声心动图?
病例摘要
女性,54岁。主因“反复咳嗽2个月余”入院。
现病史
2个多月前患者无明显诱因出现咳嗽,为刺激性干咳,偶伴少量白色黏痰,无胸闷、气喘,无胸痛,当地医院予对症治疗 (具体不详)后症状略有改善。而后行超声心动图提示左心房黏液瘤、少量心包积液。为进一步治疗来我院就诊,门诊以 “左心房黏液瘤”于2013年10月10日收入心胸外科。发病以来,患者精神、饮食尚可,无畏寒、发热,无胸痛、胸闷,无腹痛、腹胀,睡眠佳,二便正常。
既往史
个人史
生长于原籍,否认血吸虫疫水接触史,否认放射性物质接触史。否认烟、酒等特殊不良嗜好。
家族史
否认传染性疾病、遗传性疾病家族史。
体格检查
体温36.4℃,脉搏88次/分,呼吸16次/分,血压104/68mm Hg。神清,体形偏瘦。胸廓无畸形,语颤对称无增强,叩诊双肺清,听诊两肺呼吸音粗,未闻及干、湿啰音。心前区无隆起,无震颤,律齐,心前区可闻及舒张期隆隆样杂音,体位改变而杂音变化不明显,无心包摩擦音。腹部平坦,全腹软,无压痛,反跳痛。双下肢无水肿,四肢关节无红肿。
入院诊断
左心房黏液瘤。
诊断经过
入院后,血常规:白细胞计数9.01×109/L,中性粒细胞百分比73.6%,血红蛋白95g/L,血小板计数91×109/L。生化检查:乳酸脱氢酶516U/L,谷氨酰转肽酶55U/L,α-羟丁酸脱氢酶486.6U/L,总蛋白59.7g/L,清蛋白34.4g/L,总胆红素29.8μmol/L,高密度脂蛋白0.95mmol/L。凝血分析:APTT 37.6秒,PT 12.6秒, APTT-rati 1.25,PT-INR 1.09,TT15.7秒。心电图:窦性心律,ST-T改变。X线胸片:两肺纹理增强,两肺可疑小结节影。胸部CT:左心房密度不均,心脏轻度增大,心包积液,左肺感染。腹部超声:充满型胆囊结石。双肾、肾上腺超声未见明显异常。
超声心动图:左心房腔内见近圆形较低回声肿物,大小约36mm×58mm,基底部较宽,附着于左心房后壁,几乎填满整个左心房,边缘形态不规则,团块下端随心动周期较规律地在二尖瓣口稍做往返运动,舒张期几乎堵塞二尖瓣口(图80-1),该过程中团块形态变化不明显。诊断:左心房占位性病变 (性质待定),轻度主动脉瓣反流,轻-中度三尖瓣反流,中度肺动脉高压,少量心包积液。因患者左心房异常回声不均匀、边缘欠光滑且基底部较宽,仅肿物下端稍随心动周期活动,同时伴有心包积液,故考虑恶性疾病可能性大,同时左心房黏液瘤不除外,建议外科手术。
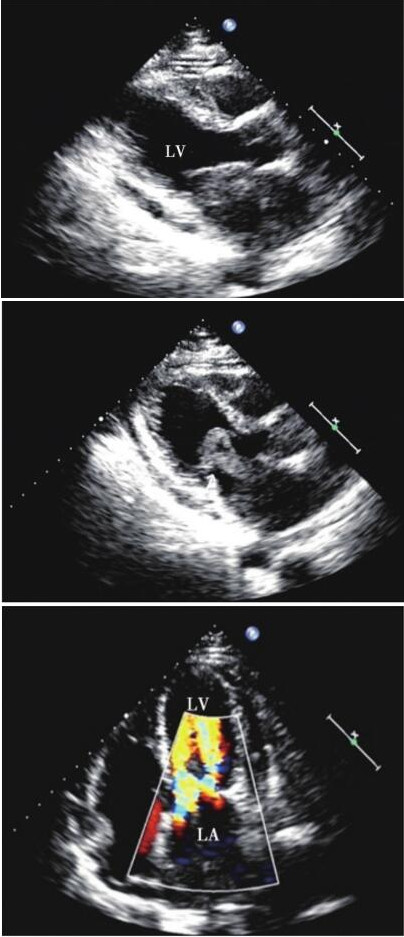
图80-1 超声心动图胸骨旁在心室长轴、心尖四腔切面
手术治疗
行手术治疗,术中探查左心房瘤体呈灰黄色肉瘤状,大小约4cm×5cm,基底部较宽,布满整个左心房后壁,向左心房、左下肺静脉开口生长,堵塞左肺静脉开口。
术后复查血常规:白细胞总数9.16×109/L,中性粒细胞百分比67.6%,血红蛋白137g/L,血小板计数380×109/L。生化检查:谷氨酸转肽酶71U/L,亮氨酸氨肽酶82U/L,总蛋白64.8g/L,清蛋白35.7g/L,尿素8.69mmol/L。心电图:V 3、V 4导联T波倒置, V1~V3导联P波倒置。X线胸片示心脏术后改变,左侧胸腔积液,右下肺模糊影。超声心动图:心脏肿瘤术后,轻-中度二尖瓣反流,左心室射血分数65%。病理报告:左心房、肺静脉恶性梭形细胞肿瘤伴大片坏死,结合免疫标记,考虑为内膜肉瘤,肿瘤大小8cm× 7cm×2cm(图80-2);免疫组化结果:SMA(3+)、CD31(散在+)、CDK4(3+)、CD34(-)、ERG(-)、Desmin(-)、H-Caldesmon(-)、S-100(-)、MDM2 (-)、CD68(-)、CD163(-)、PH H3(++)、Ki-67(约70%)。
因病理结果提示罕见恶性心脏肿瘤,请肿瘤科会诊,建议术后继续化疗减少远期复发风险,患者拒绝而要求院外休养。术后4个月,患者于当地医院复查超声心动图示左心房再次被肿瘤填充,患者拒绝进一步治疗。
最终诊断
左心房内膜肉瘤侵及肺静脉。
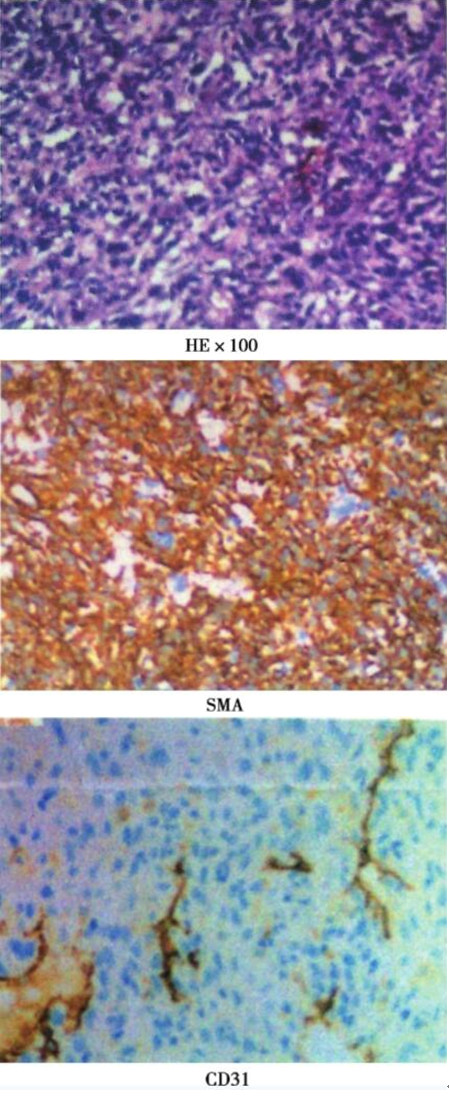
图80-2 在心室异常组织病理染色切片
病例思考
1.内膜肉瘤的临床特征是什么,如何鉴别诊断?
内膜肉瘤是一种罕见的高度恶性肿瘤,可发生在体循环、肺循环的大血管腔内,目前被认为起源于内皮下内膜间叶细胞。大部分内膜肉瘤为低分化肉瘤,免疫组织化学、电镜研究显示肿瘤呈纤维母或肌纤维母细胞分化。
本例患者在超声心动图诊断过程中主要需与黏液瘤、原发性肿瘤等鉴别,虽然超声心动图所见肿瘤下端稍有类似黏液瘤样活动征象,但该瘤体边缘形态不规则、基底过宽、瘤蒂不明显,随心动周期稍有活动过程中瘤体形态变化不明显,这些均可为临床鉴别诊断提供一定线索。
2.心脏内异常回声超声心动图鉴别诊断要点有哪些?
超声心动图作为目前常规心血管病检查手段,临床应用已被广泛认可。对于绝大多数结构性心脏病、先天性心脏病、风湿性心脏病、心肌病、心脏异常回声,心包积液、主动脉夹层等具有较高的诊断准确性,可为临床提供重要依据。超声心动图如探及心脏内异常回声,主要需考虑以下疾病。
(1)血栓:
主要超声心动图表现为心腔内团块状回声,多附于心房顶部、房室侧壁、心尖部,基底部较宽,一般无蒂,回声较强,活动度低,形态变化小。心房血栓好发于左心房,患者多有风湿性心脏病、心功能不全、心房颤动等病史,且多位于左心耳,分界清晰。心室血栓主要好发于心肌梗死患者,多位于心尖部、心室侧壁。本例患者缺乏上述基础病变,左心房内异常回声有一定活动度、回声较低、欠均匀,与血栓表现不符。
(2)赘生物:
主要附着于心脏瓣膜,也可附着于房室壁。主要超声心动图表现为瓣膜或心内膜附着一个或多个团块状回声,大小不等、形态不规则,附于瓣膜的赘生物可与瓣叶同步运动,多为中等回声,陈旧赘生物机化程度较高而回声较强,部分赘生物与瓣叶间有类似蒂样的结构。心脏瓣膜受赘生物影响可出现相对性狭窄和 (或)关闭不全。随着病情发展,赘生物可逐渐增多、增大,出现脱落、机化或钙化等改变。
(3)黏液瘤:
多发生在左心房,也可发生在右心房和右心室,左心室较少见。常规超声心动图表现为心腔内实性团块状回声,多为椭圆形或圆形;瘤体大小不一,肿块内部回声强弱不均,可见大小不等的低回声区,瘤体表面较光滑,多呈分叶状,常有蒂;瘤蒂长短粗细不一,多数附着于房间隔卵圆孔边缘,活动度较大;瘤体随心脏舒缩运动发生位置和形态改变,舒张期突入房室瓣口,收缩期纳入心房,可引起相对性房室瓣狭窄、心脏扩大。
(4)脂肪瘤:
多发生在左心室,瘤体的基底部较宽,与心室壁融合在一起,无明显界线;肿瘤所浸润的面积较大者可突向心腔内,边缘光滑,回声较强,而且活动度较小有漂浮感,无分叶。
(5)横纹肌肉瘤:
多见于婴儿、儿童,一般累及左、右心室;通常为多发性,主要见于壁内,在室间隔或左心室游离壁;肿瘤与正常心肌间有明确界限,向心腔内弧形突出;瘤体回声较强、均匀,边界清晰、规整;局部心肌可明显增厚,回声正常,无活动性或活动性小。
(6)纤维肉瘤:
多见于婴儿、儿童,通常位于左心室游离壁室间隔和心尖处;多为单发,大小不一,直径有时可达10cm;纤维瘤常见钙化,与周围正常心肌组织有明确边界。超声心动图探查显示纤维瘤多包埋于心肌内,无包膜,回声反射较心肌强,部分纤维瘤叶可向心腔内生长,导致左心室或右心室流出道梗阻。
(7)转移性肿瘤:
几乎所有全身脏器恶性肿瘤均可转移到心脏,往往作为其他脏器恶性肿瘤转移病灶的一部分,单纯转移到心脏者少见;可以是直接浸润,也可随血液或淋巴种植。超声心动图探查主要需辨别肿瘤的生长部位、浸润方式、有无邻近器官以及腔静脉、肺静脉等部位异常回声。
病例启示
内膜肉瘤是一种罕见的高度恶性肿瘤,多发生在体循环和肺循环的大血管腔内,超声心动图诊断主要需与黏液瘤、原发性肿瘤等相鉴别。该例患者并非在大血管腔内,而是在黏液瘤好发的左心房内形成附壁占位性病变,容易首先考虑黏液瘤。尽管超声可见肿瘤下端有类似黏液瘤样活动征象,但由于基底过宽、瘤蒂不明显、运动幅度小,并未形成明显“鼠窜样”活动,考虑为肿块与周围房壁组织粘连或浸润所致,且其下端轻度活动时肿块形态变化欠显著,提示该肿块质地较传统意义的左心房黏液瘤硬、弹性差,以上线索均对临床诊疗大有裨益。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








医生可以联系上你吗?我的家人和这个症状差不多
40
#心动图#
34
#左心房#
50
#罕见#
40
#心房#
38
学习了.谢谢分享
74