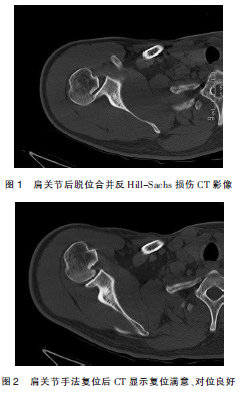
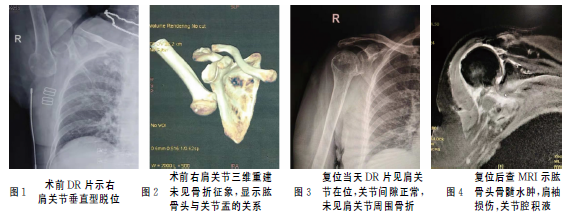
肩关节后脱位合并反Hill-Sachs损伤1例
2019-12-25 叶春晓 林志强 郭颖彬 中国骨与关节损伤杂志
肩关节后脱位在临床上较为少见,占肩关节脱位的1.5%~3.8%,其临床表现较为隐匿,容易导致漏诊,文献报道漏诊率高达60%~80%。笔者于2018-05诊治1例创伤性肩关节后脱位合并反Hill-Sachs损伤,分析此类损伤的早期诊断及处理方法,为避免其漏诊、误诊提供临床参考,报道如下。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#后脱位#
40
#反Hill-Sachs损伤#
27
#肩关节#
37
#损伤#
28
#脱位#
37
谢谢了学习了
90