JBJS:多关节置换肺栓塞和死亡风险**
2013-12-27 xm174cxy dxy
每年美国的全髋(THA)和全膝关节置换(TKA)手术超过100万例,在关节置换手术的诸多并发症中,肺栓塞只占其中不到1%。虽然可以通过各种手段进行预防,但如果一旦发生就可能使患者致残甚至死亡。目前在美国接受初次择期关节置换的住院患者中肺栓塞的发生率尚不清楚。为了明确初次择期THA和TKA住院患者肺栓塞的发生率及危险因素,来自马里兰大学医学院的Zahir等对1998-2009年Healthcare
每年美国的全髋(THA)和全膝关节置换(TKA)手术超过100万例,在关节置换手术的诸多并发症中,肺栓塞只占其中不到1%。虽然可以通过各种手段进行预防,但如果一旦发生就可能使患者致残甚至死亡。目前在美国接受初次择期关节置换的住院患者中肺栓塞的发生率尚不清楚。为了明确初次择期THA和TKA住院患者肺栓塞的发生率及危险因素,来自马里兰大学医学院的Zahir等对1998-2009年Healthcare Cost and Utilization Project(HCUP)全国患者的数据进行回顾性队列研究,其结果发表于2013年11月20日JBJS 95期22卷上
对象为60岁以上接受择期初次全髋或全膝关节置换的病例,排除标准包括:既往髋关节手术史及创伤等。研究的变量包括:THA、TKA、或双关节置换(双髋、双膝或一髋和一膝),研究的主要结局为肺栓塞,协变量包括:年龄(75岁以上或75岁以下)、性别、种族(白种人或非白种人)、手术指征(骨关节炎、风湿性关节炎、骨坏死)、Charlson合并症指数和房颤。
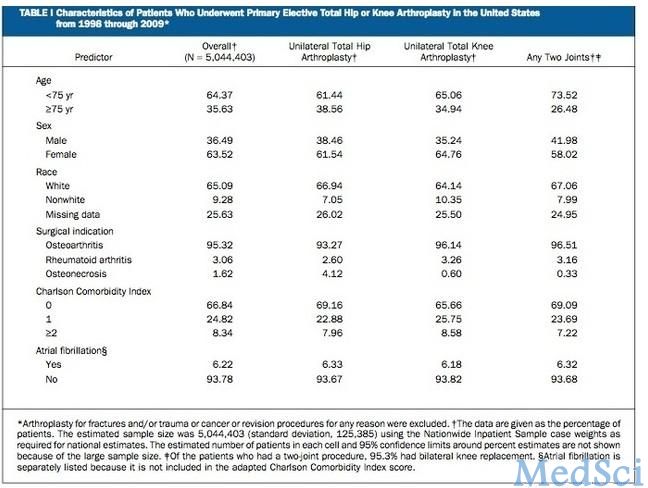
共纳入5,044,403例初次THA或TKA病例(表1),其中TKA占66%,同时行两种关节置换手术的不到5%,这其中95.3%为双侧TKA。95.3%病例的手术原因为骨关节炎。75岁以下病例在将近2/3,女性占2/3,白种人占2/3,66.8%的病例没有合并症。和单关节置换相比,双关节置换的病例更年轻、健康状况更好、男性的比例更高,其中有将近70%的病例没有并发症。全部病例中合并房颤的只占6.22%。
表1择期初次THA和TKA的病历资料
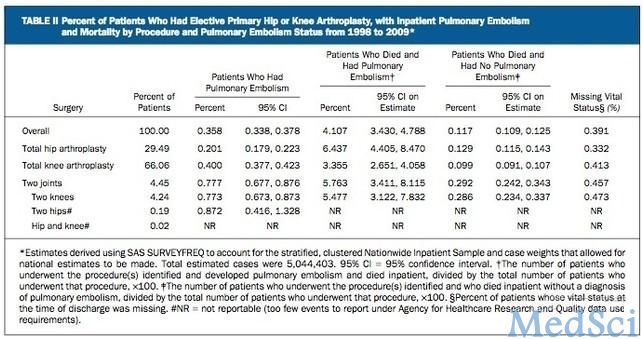
未经校正的住院期间肺栓塞总发生率为0.358%(表2)。单侧TKA住院病例肺栓塞的发生率(0.400%)是单侧THA病例(0.201%)的2倍,多关节置换肺栓塞的发生率(0.777%)是单关节置换的4倍,双侧TKA肺栓塞的发生率(0.773%)是单侧TKA的2倍。
表2 择期初次THA和TKA肺栓塞的发生率及死亡率
双侧THA肺栓塞的发生率(0.872%)要高于双侧TKA(0.773%)。单侧THA合并单侧TKA因数量较少无法估计肺栓塞的发生率。
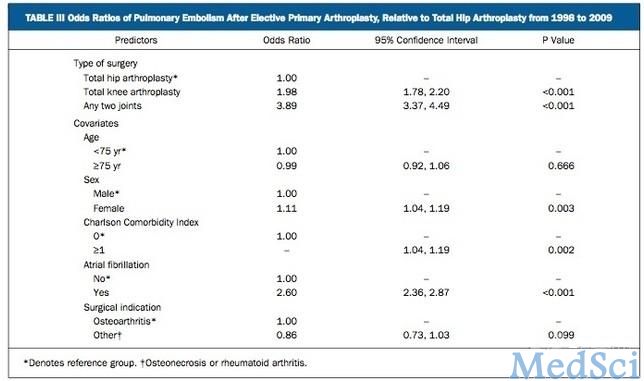
考虑了年龄、性别、Charlson合并症指数、房颤、手术指征等因素,接受双关节置换手术发生肺栓塞校正后的相对危险度(OR值)比全髋关节置换术高3.89倍(表3)。
研究者据此认为:择期全膝关节置换术的住院患者肺栓塞的发生率高于全髋关节置换术,而多关节置换肺栓塞和死亡风险最高。
原文出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#置换#
27
#死亡风险#
34
#JBJS#
30