Exp Lung Res:肺动脉ERK表达或与吸烟者PASMC的异常增殖相关
2013-06-20 Exp Lung Res dxy
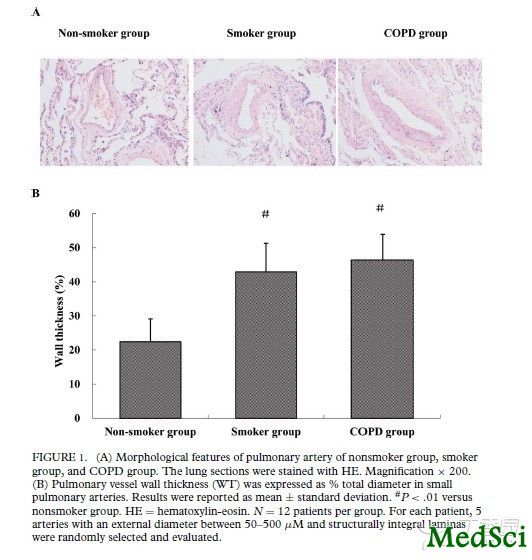
A图示:非吸烟组、吸烟组、及COPD组肺动脉的形态学特征。B图示:非吸烟组、吸烟组、及COPD组小肺动脉血管壁的厚度,以血管直径的百分比表示。 吸烟可能会促进慢性阻塞性肺疾病(COPD)患者肺动脉高压的形成,而肺血管重塑、及与之相关的肺动脉平滑肌细胞(PASMC)的增殖可能参与了这一过程。但迄今为止,人们对于上述过程中所存在的分子机制仍然知之甚少。 为了探讨在肺功能正常的吸烟者、以及患有轻
A图示:非吸烟组、吸烟组、及COPD组肺动脉的形态学特征。B图示:非吸烟组、吸烟组、及COPD组小肺动脉血管壁的厚度,以血管直径的百分比表示。
吸烟可能会促进慢性阻塞性肺疾病(COPD)患者肺动脉高压的形成,而肺血管重塑、及与之相关的肺动脉平滑肌细胞(PASMC)的增殖可能参与了这一过程。但迄今为止,人们对于上述过程中所存在的分子机制仍然知之甚少。
为了探讨在肺功能正常的吸烟者、以及患有轻度至中度COPD的吸烟者的肺动脉中,细胞外信号调节激酶(ERK)所起的作用,来自我国卫生部呼吸疾病重点实验室,华中科技大学同济医学院呼吸和重症医学科的徐永健及其同事开展了一项研究,研究结果在线发表于2013年4月24日的《实验肺脏研究》(Experimental Lung Research)杂志上。研究结果显示:肺动脉ERK表达的增加,可能与吸烟者PASMC的异常增殖机制有关。而且这种相关性不受吸烟者是否伴有COPD的影响。
该研究中所用的肺外周组织,分别来自14名肺功能正常的非吸烟者、18名肺功能正常的吸烟者、和16名患有轻度至中度慢性阻塞性肺病的吸烟者。研究者通过苏木精-伊红(HE)染色观察了所取得肺动脉的形态学改变;并将原代培养的人肺动脉平滑肌细胞(HPASMC)暴露于香烟烟雾提取物(CSE)中。随后,研究者采用细胞计数及四甲基偶氮唑蓝(MTT)法测定了相关细胞的增殖状况,并使用蛋白印迹法分析了ERK蛋白的表达状况。
该研究的主要结果为:形态计量学分析表明,与不吸烟者相比,吸烟组和COPD组受试者肺血管壁的厚度明显增加(P<0.01)。同样,吸烟组和COPD组受试者的ERK蛋白水平较不吸烟组受试者也有显著增加(P<0.01)。当使用5%CSE处理相关的HPASMC细胞后,后者的ERK的蛋白表达水平明显增加(P<0.01),并大大促进了HPASMC的细胞增殖(P<0.01)。
该研究结果显示:肺动脉ERK表达的增加,可能与吸烟者PASMC的异常增殖机制有关。而且这种相关性不受吸烟者是否伴有COPD的影响。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#PASMC#
37
#ERK#
35
#SMC#
39
#吸烟者#
38