 |
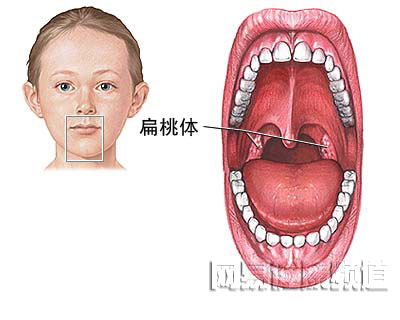
| 扁桃腺位于喉后部,内含抗感染的免疫细胞。 |
 |
|
当出现下述情况时,则应考虑进行扁桃体切除术:扁桃腺炎频繁发作,或者扁桃腺炎严重影响到健康或使儿童停学、以及影响听力或呼吸时。然而,有时扁桃腺切除术不一定非作不可的,这要根据实际情况进行相应的分析处理。 扁桃腺切除术适应症: ·扁桃腺炎一年发作5次或5次以上 ·扁桃腺炎两年内每年发作3次或3次以上 ·扁桃腺肿大引起上呼吸道阻塞 ·扁桃腺脓肿周期性发作 |
 |
| 手术在全麻下进行,手术医生会将患者张口,把舌头往前拉以显示扁桃体。然后,把扁桃体后推切除。大多数情况下手术伤口是无需缝合的。 |
 |
| 术后一般观察24小时则可出院。通常情况下扁桃腺切除不会对以后的生活有任何不良影响。 |
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#扁桃体切除术#
48
#切除术#
35
#扁桃体切除#
47