Gastroenterology:他汀类药物在结肠癌患者生存中的应用
2017-05-14 zhangfan MedSci原创
他汀类药物与结肠癌风险降低相关,对于BMP通路完整或KRAS突变患者其效果更为显著,该结果还需要进一步的临床试验确证
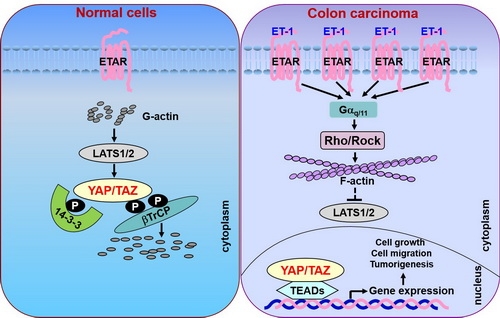
模型研究发现他汀类药物通过抑制Ras信号并激活骨形态发生蛋白(BMP)信号通路,降低结直肠癌的发病率,提高结肠癌患者的生存率。近日研究人员就他汀类药物对结肠癌患者总生存期的影响以及相关信号通路的作用进行了研究。
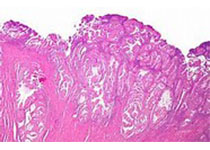
研究数据来自PHARMO 数据库,其中包括2002年至2007年间荷兰结肠癌患者资料获得999份结肠癌标本的组织芯片。采用多变量泊松回归生存模型和COX分析研究他汀类药物对患者生存的影响,对肿瘤组织Smad4,BMPR1A,BMPR1B BMPR2蛋白水平通过免疫组化分析。主要终点指标为总死亡率和癌症特异性死亡率。
在999例患者中,有210名(21.0%)的患者在确诊结肠癌后服用了他汀类药物。研究发现,他汀类药物与降低全因死亡风险显著相关(相对风险[RR], 0.67; 95% CI, 0.51–0.87; P=0.003),与降低癌症死亡率相关(RR, 0.66; 95% CI, 0.49-0.89; P=0.007),对于肿瘤组织BMP信号完整的患者,他汀类药物可降低其死亡风险(RR, 0.39; 95% CI, 0.22–0.68; P=0.001),对于BMP信号突变患者,药物作用不显著( RR, 0.81; 95% CI, 0.55–1.21; P=0.106; P<0.0001 )。相比于KRAS未突变患者,药物对突变患者作用显著(KRAS未突变:RR, 0.81; 95% CI, 0.56–1.18; P=0.273,KRAS突变:RR, 0.59; 95% CI 0.35–1.03; P=0.062; )。
研究认为,他汀类药物与结肠癌风险降低相关,对于BMP通路完整或KRAS突变患者其效果更为显著,该结果还需要进一步的临床试验确证。
原始出处:
Philip W. Voorneveld et al.Statin Use After Diagnosis of Colon Cancer and Patient Survival. Gastroenterology. May 13 2017.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Gastroenterol#
24
#GAS#
29
#AST#
32
#患者生存#
27
#他汀类药#
30
学习了,谢谢
54
#Gastroenterology#
22
这个应用还是挺不错的
52
结肠癌治疗的进步
52
免疫组化为啥只研究了这几个指标?
57