Nat Chem:研究人员开发出阻断感冒病毒的新分子
2018-05-16 Tierna 生物探索
据5月14日Nature子刊上的最新研究,科学家已开发出一种新的药物分子,可以通过防止病毒劫持人类细胞来完全阻断引起感冒的病毒。测试表明,这种新分子除可防止多种感冒病毒在细胞中复制之外,还可以有效对抗包括脊髓灰质炎病毒和引起口蹄疫的病毒等其他病毒。
伦敦帝国学院(Imperial College)化学系的Edward Tate博士领导的科学家们在《Nature Chemistry》杂志以一篇题为“Fragment-Derived Inhibitors of Human N-Myristoyltransferase Block Capsid Assembly and Replication of the Common Cold Virus”的论文中报告了他们的进展。DOI:10.1038/s41557-018-0039-2
1感冒罪魁祸首——鼻病毒
鼻病毒(rhinovirus)属于小RNA病毒科(Picornaviridae,包括脊髓灰质炎病毒、口蹄疫病毒、柯萨奇病毒、甲型肝炎病毒和肠道病毒71型等病原体)。目前针对感冒的疗法只能缓解症状,并不能预防或治疗病毒感染。这既是因为引起感冒的鼻病毒有超过100种不同的变体(这阻止了广谱疫苗的开发),也是因为用直接靶向鼻病毒的药物治疗时,该病毒能够快速发生突变。
Tate博士说:“普通感冒对我们大多数人来说只是一种不便,但对患有哮喘和慢性阻塞性肺疾病(chronic obstructive pulmonary disease ,COPD)的人来说可能会引起严重的并发症。如果在感染初期服用治疗药物,可能会非常有益,我们正在研制一种可以吸入的药物,以便迅速进入肺部。”
2发现抗鼻病毒靶标
鼻病毒衣壳的组装依赖于N-肉豆蔻酰转移酶(N-myristoyltransferase,NMT,一种人类酶)的活性,其通过被称为肉豆蔻酰化的过程对病毒衣壳蛋白之一VP0进行修饰。人NMT以NMT1和NMT2两种形式存在,以前对脊髓灰质炎病毒的研究表明,NMT是衣壳复制和传染性的先决条件。“因此,宿主NMT可能是一种有吸引力的抗病毒药物靶标,因为宿主NMT是病毒复制中的不变因素。”作者说。
虽然帝国理工学院的研究人员以前已经生成了NMT抑制剂,但迄今为止,这些分子主要是针对原生动物寄生虫或真菌中的NMT而开发的,它们只“适度地”降低了人类酶的活性。作者解释道:“我们推断,一个针对人NMTs的优化新系列可以大大提高细胞活性,并且可以用来探索NMT抑制的抗病毒潜力。”
当研究人员调查针对人类疟疾寄生虫NMT的高通量化合物筛选的潜在影响时,这个机会出现了。他们鉴定了一种对人NMT 1(HsNMT1)有一定活性的化合物,并以此为起点开发了一种更有效的分子,该分子可以抑制人NMT 1和NMT 2(HsNMT1/2)酶。
3最有效的人NMT抑制剂
这一设计过程利用了他们所描述的“不寻常的片段重建方法”,科学家通过这种方法构建了具有“显着的协同抑制效应和互补结合模式”的片段状化合物,然后将它们连接在一起,产生了最有效的人NMT抑制剂,被命名为IMP-1088。
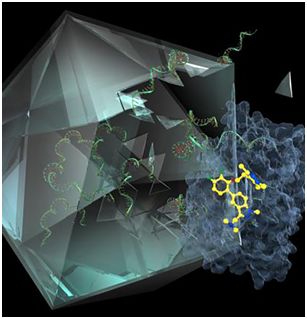
The novel molecule IMP-1088 (yellow) blocks human NMT (blue), a protein essential for the cold virus to assemble the geometric capsid "shell" that encloses its RNA genome (green). [Imperial College London]
初步研究证实IMP-1088阻断了人细胞中鼻病毒衣壳的加工。使用IMP-1088及其效力较弱的类似物也阻断了人细胞中传染性小RNA病毒的产生,并保护细胞免受病毒诱导的细胞毒性。令人鼓舞的是,IMP-1088对一系列鼻病毒血清型以及对小RNA病毒PV和FMDV也表现出强有力的抗病毒作用。
IMP-1088还阻断了人支气管上皮细胞中的病毒复制,研究人员称这是一种更能代表人类感染的模型。IMP - 1088的作用甚至在吸入皮质类固醇丙酸氟替卡松(corticosteroid fluticasone proprionate,用于治疗COPD和哮喘患者)的联合给药期间也得以维持。
值得一提的是,IMP-1088即使在感染后3小时内也能显着抑制传染性病毒的产生,这表明该抑制剂即使在主动感染的情况下也能保持效力。此外,该结果还强烈表明VP0肉豆蔻酰化是产生传染性鼻病毒颗粒的必要条件。
在最后一组实验中,研究小组证明阻断NMT可以防止病毒粒子的聚集。有趣的是,他们指出,IMP-1088并没有阻止病毒RNA的产生或鼻病毒多蛋白的翻译。 “这些数据表明,介导NMT抑制剂有效性的关键步骤是蛋白质翻译和感染性病毒粒子的产生。” 研究人员说。
4研究意义
最后,作者总结道:“许多小RNA病毒已经进化成依赖于宿主肉豆蔻酰化的观察结果表明,这种作用模式可能会绕过针对NMT的药物的耐药性的发展,因为病毒突变不会影响针对宿主酶的抑制剂效力。此处提供的数据表明,人NMT作为肉豆蔻酰化依赖性小RNA病毒感染的药物靶标值得进一步研究,它在治疗鼻病毒诱导的哮喘、COPD、囊性纤维化和其他小RNA病毒疾病的恶化中具有潜在的应用前景。”
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#阻断#
35
#Nat#
34
#研究人员#
32
#新分子#
38
可以开发新药
58