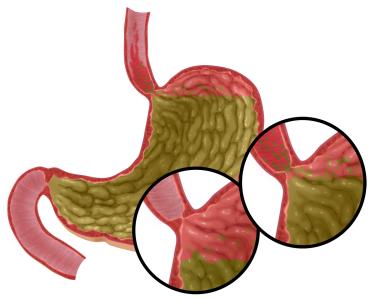
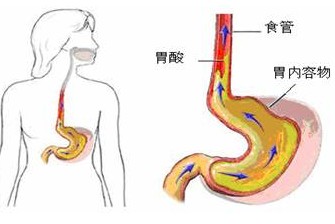
胃食管反流疾病
2017-09-15 MedSci MedSci原创
食管腺癌(EA)是一种越来越常见的癌症,它会悄无声息地影响食管--将食物送入胃的肌肉管。引起EA的原因并不为人所知,但胃食管反流疾病(GERD),其特征是慢性胃灼热和胃酸反流,是已知最强烈的危险因素。现在在《科学报告》杂志亚历山大·齐卡(Scientific Reports)博士和同事们发现,酸性胆汁反流引起的食道细胞DNA损伤(BA / A)会激活线粒体(细胞动力室)中称为NADPH氧化酶的酶,
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#胃食管#
25
#胃食管反流#
34
#食管#
32
#反流#
26
学习了
46
胃食道反流病.学习了.
39
学习了.谢谢分享
45
不错的文章值得学习
47
学习了.涨知识了!
55
Emmmmmmm.学习了
27