盘点:近期胃食管反流研究进展一览
2017-03-03 MedSci MedSci原创
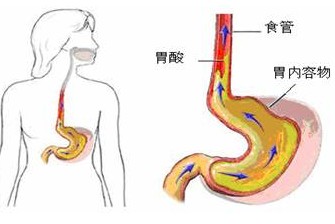
胃食管反流病(GERD),是一种极为常见的疾病,在西方国家成人中的发病率为10%-20%。越来越多的研究已经证明了身体质量指数增加和胃酸反流症状恶化之间的直接联系。胃食管反流患可能会影响越来越多的人。随着肥胖情况日益严重严重,胃食管反流病可能更加流行。尽管治疗胃食管反流病的非处方疗法很多,持续或预警症状应始终及时咨询医生。本文小编汇总了近期胃食管反流亮点研究,与大家分享。【1】Stretta射
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#胃食管#
22
不断学习不断进步
48
继续努力锲而不舍
68
不断学习不断进步
69
不断学习不断进步
56
胃食管反流的新进展
0
继续努力锲而不舍
18
胃食管反流的新进展
30
胃食管反流的新进展
31
学海无涯苦作舟
19