Hepatology:急性肝衰竭的出血并发症
2018-04-24 MedSci MedSci原创
尽管有明显的出血症状,但ALF患者发生临床上明显的出血并不常见;ALF患者的出血并发症是全身严重炎症的标志,而不是凝血障碍疾病,提示预后不良。
研究背景和目的:急性肝功能衰竭(ALF)患者中,凝血酶原时间升高和血小板减少可能会导致出血。然而,出血并发症的发生率、部位、危险因素和临床意义尚未在ALF患者中得到量化。
研究方法:该研究调查了1998年至2016年间,参与ALF研究小组的1770例成年患者。入院后7天调查出血并发症及输血情况。评估出血并发症与21天死亡率的关系。
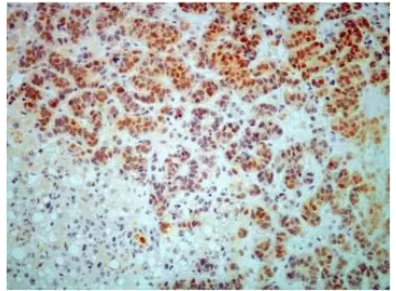
研究结果:尽管国际标准化比率为2.7,血小板计数为96 x 10(9) /L,但只有187例患者出现出血并发症(11%),包括173例自发出血和22例术后出血。84%的自发性出血事件来自上消化道,很少导致输注红细胞。20例患者发生颅内出血;其中一半是自发的,一半是在颅内压监测后。是死亡率分别为20%和50%的原因。出血患者和接受红细胞输入的患者更严重的疾病是肝外器官系统衰竭,而不是肝细胞衰竭。与此相一致的是,出血并发症与血小板数量减少有关,与国际标准化比值较高无关。任何血液成分的输血与第21天几乎增加的2倍死亡率、需要进行的肝移植相关,但出血并发症仅占死亡原因的5%。
研究结论:尽管有明显的出血症状,但ALF患者发生临床上明显的出血并不常见;ALF患者的出血并发症是全身严重炎症的标志,而不是凝血障碍疾病,提示预后不良。
原始出处:
Stravitz RT, Ellerbe C, Durkalski V, et al. Bleeding complications in acute liver failure. Hepatology, 2018, 67(5), 1931-1942. doi: 10.1002/hep.29694.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#并发#
30
#肝衰#
30
#急性肝衰竭#
35
#EPA#
26
学习了很有用
59