病例分享:心梗可不止会胸闷痛,这种情况你想到没?
2018-03-22 作者:王加伟 单位:惠州市第一人民医院 循环界
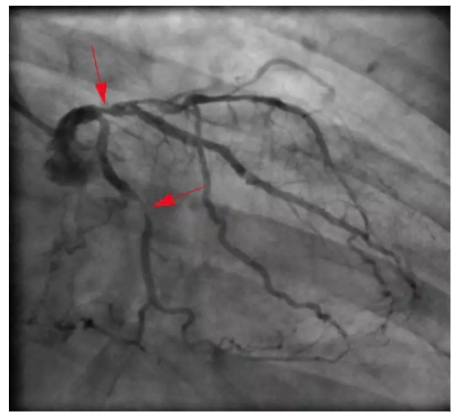
73岁男性,反复头痛6个月,劳累或受凉后诱发,休息后头痛通常会迅速缓解。6周前头痛再发加重,频率增加,较低水平活动可发生。同时运动中出现轻微胸痛,然而头痛更明显。既往有2型糖尿病病史10年,无周围神经病变或视网膜病变,仅有轻度肾损害(eGFR 50 mL/min/1.73 m2)。有创伤性硬膜下出血手术史6年,术后2年经磁共振明确诊断为脑梗死。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#胸闷#
26
很好的文章.好好学习
65
非常精彩的病历.获益匪浅.谢谢!
65
了解一下.谢谢分享!
65
阅
78