肿瘤细胞的异质性决定了它的侵袭能力!
2016-08-20 佚名 来宝网
由Bellvitge生物医学研究所(IDIBELL)表观遗传学和癌症生物学计划(PEBC)的主任Manel Esteller博士、ICREA研究员和巴塞罗那大学(UB)的遗传学教授领导的一项新研究发现,大肠肿瘤表现出涉及到该病临床过程的后生异质性。描述这一发现的论文已经发表在《胃肠病学》杂志上。 人类肿瘤在患者体内以指数速率增长,这意味着,它们也必须适应环境的变化并存活下来,如化疗或放疗带来

由Bellvitge生物医学研究所(IDIBELL)表观遗传学和癌症生物学计划(PEBC)的主任Manel Esteller博士、ICREA研究员和巴塞罗那大学(UB)的遗传学教授领导的一项新研究发现,大肠肿瘤表现出涉及到该病临床过程的后生异质性。描述这一发现的论文已经发表在《胃肠病学》杂志上。
人类肿瘤在患者体内以指数速率增长,这意味着,它们也必须适应环境的变化并存活下来,如化疗或放疗带来的环境变化。这种能力的一部分被认为是由于肿瘤内存在不同类型的癌细胞:此概念被称为异质性。
在这个意义上说,关于这个问题的第一个研究,是在肿瘤内水平上发现了一些不同的遗传病变的存在。然而,表观遗传变化,即基因活性的变化也可以是异质的。基因的活性更加具有动态性。
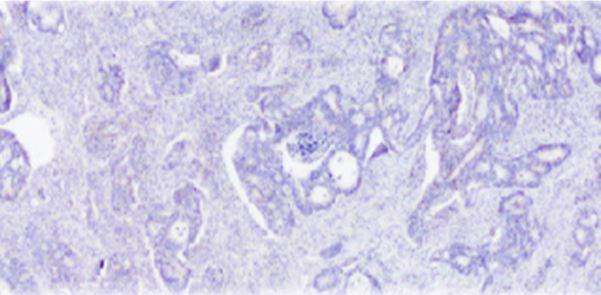
“在大肠癌患者中,我们确定了每个肿瘤的三个区域的表观基因组。消化道起始处、中央和生长进入血管处,表明了肿瘤内的异质性的存在,这意味着每个区域都存在差异,“马内尔博士解释说:“表观遗传学差异更大的区域是侵入性肿瘤的前部,即与邻近的正常组织相互作用的区域。我们也看到,肿瘤内与转移阶段最相似的是肿瘤中最老的部分,这表明即使在很早期,肿瘤已经开始传播。”
在后生水平上的瘤内异质性也可具有预测作用,Esteller博士补充说:“此外,数据显示,三个区域的相似度越高,肿瘤的侵略性越强,就好像具有更强增殖能力的肿瘤细胞群已经被选出来了一样。测量肿瘤分子异质性的水平可以作为预后和对某些疗法的抗性的预测因子。”
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









这篇资讯写的真好,带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
63
这篇资讯写的真好,带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
51
#肿瘤细胞#
26
可否提供更详细的论文信息,方便查找,进一步学习
59
学习了!!??
63
阅读了。
60
学习起来
24