Stroke:短暂性脑缺血发作中孤立性非典型短暂性症状的临床意义!
2017-05-10 xing.T MedSci原创
由此可见,短暂性缺血发作的诊断应考虑和研究孤立性非典型TS患者。
与典型的短暂性症状(TS)相反,非典型的TS,如局部感觉障碍、构音障碍、眩晕、步态不稳、不寻常的皮层视觉缺失、复视,通常不被归类为短暂性脑缺血发作的症状,当它们单独发生时,其临床意义经常被否认。
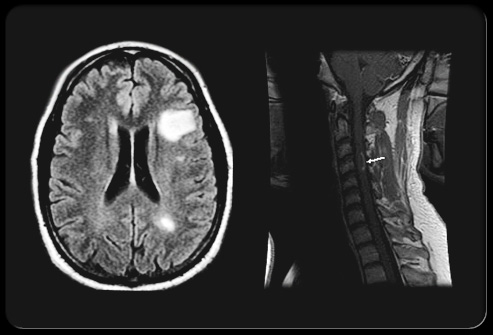
近日,卒中领域权威杂志Stroke上发表了一篇研究文章,研究人员对其所在的短暂性脑缺血发作诊所(2003-2008年)连续就诊的近期TS患者进行了系统的脑、动脉和心脏检查。在排除主要鉴别诊断后,研究人员比较了孤立的典型或非典型TS患者和非孤立的TS患者脑成像图像上近期脑梗死的患病率、主要调查结果(症状性颅内或颅外动脉狭窄≥50%、颈动脉夹层和主要来源于心脏的栓塞)和主要血管事件的1年风险。
在1850例可能或明确的缺血性诊断患者中,有798例(43.1%)患者为孤立性TS:621例为典型TS患者(33.6%)和177例为非典型TS患者(9.6%)。脑成像图像上急性脑梗死发生情况在孤立的非典型TS患者和典型TS患者之间类似,但是比非孤立的TS患者更不频繁,观察的发生率分别为10%、11.5%和15.3%(P<0.0001)。主要调查结果分在18.1%、26.4%和26.3%的患者中可以观察到(P=0.06)。3组间大血管事件的1年风险差异无统计学意义。
由此可见,短暂性缺血发作的诊断应考虑和研究孤立性非典型TS患者。
原始出处:
Philippa C. Lavallée,et al. Clinical Significance of Isolated Atypical Transient Symptoms in a Cohort With Transient Ischemic Attack.Stroke. 2017. https://doi.org/10.1161/STROKEAHA.117.016743
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#短暂性脑缺#
21
#短暂性#
21
#脑缺血#
26
#非典型#
22
#孤立性#
33
学习了……厉害几次
49
非常不错!学习了
43
谢谢分享,学习了
50
学习了,谢谢分享
37
短暂脑缺血发作,应引起重视。
44