Cell:鉴别出参与细胞信号转导的特殊“巨大复合物”
2016-08-08 佚名 生物谷
一项刊登在国际杂志Cell上的研究报告中,来自杜克大学医学中心等机构的科学家通过研究揭开了细胞产生信号机制的新信息,该研究或有望帮助指导特殊药物疗法的开发。多年以来,科学家们已经通过研究阐明了在接受来自激素、神经递质甚至药物的化学信号后细胞改变功能的分子机制,细胞外部的受体被认为可以发起信号产生的过程,从而提醒蛋白诱发级联反应事件引发所期望产生的反应。然而近些年来,该过程表现出了额外的复杂性,这
一项刊登在国际杂志Cell上的研究报告中,来自杜克大学医学中心等机构的科学家通过研究揭开了细胞产生信号机制的新信息,该研究或有望帮助指导特殊药物疗法的开发。多年以来,科学家们已经通过研究阐明了在接受来自激素、神经递质甚至药物的化学信号后细胞改变功能的分子机制,细胞外部的受体被认为可以发起信号产生的过程,从而提醒蛋白诱发级联反应事件引发所期望产生的反应。然而近些年来,该过程表现出了额外的复杂性,这些复杂性开始“公然挑战”基本的假设,值得注意的就是细胞内部信号产生的机制到底是怎么样的?
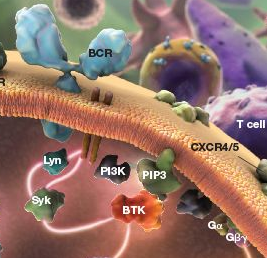
这项研究中,研究者Robert Lefkowitz表示,我们似乎就可以揭开其中的奥秘所在。文章中我们描述了一种新型模式,即名为G蛋白偶联受体(GPCRs)的一类细胞表面受体如何激活细胞的信号机制。我们都知道,细胞内部质膜上的GPCRs可以激活G蛋白表达,随后G蛋白就可以作为分子开关来讲细胞外部的信号传输到细胞内部,告知细胞该如何发挥作用。该激活过程会随着脱敏作用而发生,其通过β-抑制蛋白结合到特殊受体上来完成,而且这种激活作用会阻断后期G蛋白的激活并且将受体内陷到细胞中(或吞噬作用),这两种过程的最后结果就是沉默受体信号,使得细胞功能恢复现状。
近些年来,研究者发现,某些GPCRs可以持续向G蛋白发送信号,甚至是在β-抑制蛋白被破坏以及受体发生内陷的情况下;这项研究中研究者就利用生物化学、生物物理学等一系列技术描述了此前一种未知的受体超结构的存在、功能及架构特性,研究者将其称之为“巨大的复合物”(mega-plexes),这种特殊的复合物不同于受体和β-抑制蛋白的典型偶联,其可以通过核心区域及尾部区域同时与G蛋白和β-抑制蛋白同时结合,由于β-抑制蛋白只能够同受体尾部相互作用,当受体整个内表面暴露时,就可以使受体维持对G蛋白的激活作用。
研究者Lefkowitz说道,这种特殊的巨大复合物的形成就可以帮助解释G蛋白如何被GPCRs纳入后还可以持续发送信号,这就为我们后期有效控制来自细胞内外部的信号分子来进行新型疗法的开发提供了新的思路;此前研究结果表明,当G蛋白信号在不同的细胞腔隙中发生时,细胞往往会产生不同的反应。
因此如果研究者能够调节特殊细胞腔隙中的信号,或许就能够开发出治疗特殊疾病且不产生任何副作用的新型药物,最后研究者指出,当然这项研究目前仅处于初期研究阶段,其距离临床应用的路还非常遥远,当然我们后期还将进行更加深入的分析和研究。
原始出处
Alex R.B. Thomsen8, Bianca Plouffe8, Thomas J. Cahill III8, Arun K. Shukla9, Jeffrey T. Tarrasch, Annie M. Dosey, Alem W. Kahsai, Ryan T. Strachan, Biswaranjan Pani, Jacob P. Mahoney, Liyin Huang, Billy Breton10, Franziska M. Heydenreich11, Roger K. Sunahara, Georgios Skiniotis, Michel Bouvier, Robert J. Lefkowitz.GPCR-G Protein-β-Arrestin Super-Complex Mediates Sustained G Protein Signaling.Cell.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#细胞信号转导#
36
#CEL#
27
#Cell#
22
#复合物#
37