葛均波院士:经导管主动脉瓣置换,正向精细化发展
2016-12-12 中国医学论坛报今日循环 复旦大学附属中山医院心内科 潘文志 周达新 葛均波(转载需授权) 中国医学论坛报今日循环 潘文志
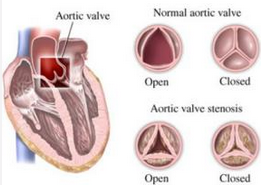
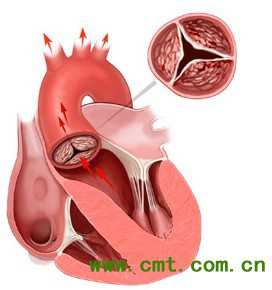
无可奈何花落去,似曾相识燕归来。新年的钟声即将敲响,又到了辞旧迎新的时刻。经过12年的成长,经导管主动脉瓣置换(TAVR)已经从一个呱呱坠地的婴儿成长为一个青春洋溢的少年。 国际上TAVR目前已发展的相当成熟,正向精细化发展。回顾本年的文献,可发现许多研究都是针对TAVR的技术细节或者特定的临床问题进行深入探讨,而不是之前那样从总体上观察技术的效果、死亡率及并发症等。本年度发表TAVR
无可奈何花落去,似曾相识燕归来。新年的钟声即将敲响,又到了辞旧迎新的时刻。经过12年的成长,经导管主动脉瓣置换(TAVR)已经从一个呱呱坠地的婴儿成长为一个青春洋溢的少年。
国际上TAVR目前已发展的相当成熟,正向精细化发展。回顾本年的文献,可发现许多研究都是针对TAVR的技术细节或者特定的临床问题进行深入探讨,而不是之前那样从总体上观察技术的效果、死亡率及并发症等。本年度发表TAVR研究数量很多,本文只对重要进展进行盘点。
中危患者,获强证据
公布于美国心脏病学会(ACC)2016年科学年会的PARTNER 2A试验,是TAVR领域本年度最重磅的研究[1]。
研究纳入2032例外科手术中危、严重主动脉狭窄患者,根据患者临床特征及影像检查将其分为股动脉(76.3%)或经胸腔入路组(23.7%),然后每个组再随机分组进行TAVR(使用Sapien XT 瓣膜)或外科瓣膜置换术(SAVR)治疗。研究终点为死亡或致残性卒中发生率。
结果显示,使用意向治疗分析,TAVR组与SAVR组的2年时主要终点发生率分别为19.3%与21.1%(HR = 0.89; 95% CI, 0.73-1.09; 非劣效性P = 0.001);使用符合方案集分析,两组主要终点发生率分别为18.9%与21.0%(HR = 0.87; 95% CI, 0.71-1.07; 非劣效性P < 0.001)。在股动脉入路组,TAVR主要终点发生率更低(HR= 0.79; 95% CI, 0.62-1);而经胸腔组患者两者治疗方法并无差别。
研究还发现,TAVR组患者的主动脉瓣面积更大,急性肾损伤、严重出血及新发房颤发生率更低,而外科治疗组的严重血管并发症及主动脉瓣周漏发生率更低。本试验的主要结论是中危患者中TAVR在的效果不劣于外科治疗,在股动脉入路亚组中,TAVR甚至优于外科治疗组。
Thourani VH[2]使用倾向评分匹配的方法,将SAPIEN 3中危组队列研究(iS3)的数据与PARTNER 2A试验的数据进行集中分析。iS3研究中,共入选1077 例外科手术中危的患者;而PARTNER 2A试验中,纳入了963例TAVR者(使用的是SAPIEN XT瓣膜)和747例SAVR者。倾向评分匹配分析显示,TAVR组(iS3 +PARTNER 2A)的主要复合终点(死亡+卒中+中重度主动脉瓣反流)发生率低于SAVR者(PARTNER 2A)。研究结论是,对于外科手术中危患者,TAVR可能是优于SAVR的治疗选择。
在CoreValve High Risk 研究中,原本均要选高危的患者,但最终部分的中危患者也被入选到该研究中。2年随访的时的亚组分析显示,在STS≥7分的亚组,TAVR的全因死亡和SAVR无差异,而STS<7分亚组,TAVR的全因死亡低于SAVR组(15% vs 26.3%,P<0.01)[3]。该研究结果也为外科手术中危患者的TAVR提供有力证据。
然而,2016年美国心脏学会(AHA)科学年会公布的GARY 中危患者研究的结果与以上研究有所不同。本次研究主要对比真实世界中中度外科手术风险的严重主动脉瓣狭窄患者,接受TAVR或SAVR治疗两组的基线特征及术后临床效果。结果显示:1年随访时,TAVR组死亡率更高(16.6% VS 8.9%,P<0.001);在使用倾向得分匹配进行校正后,TAVR组的死亡率仍较SAVR组偏(15.52% vs 10.89%,P=0.002)。
应该来说,GARY研究作为真实世界的研究,具有一定的意义。首先,它揭示了真实世界中接受TAVR或SAVR患者的特征。可以看出,与SAVR组比,TAVR组年龄更高、病情更危重。这提示,在实际临床实践中,对于病情更危重、年龄更高的中危患者,临床实践倾向于选择TAVR而不是SAVR,这显示医师和患者对TAVR的信任。本研究显示1年随访时TAVR组死亡率更高。
对于这个结果,要谨慎看待。首先,本研究是注册研究,并非严格随机对照研究,其结果也就缺乏说服力。其次,住院期间及1个月随访时,两组全因死亡率差异并非很显著,这说明TAVR具有不劣于SAVR的安全性。即使采用倾向得分匹配进行校正,分析结果仍存在较大缺陷,有些因素混杂作用并非线性的,难以被准确校正,而许多潜在的混杂因素可能还没被校正。
多种路径,百花齐放
TAVR目前最主流路入途径为经股动脉,其次是经心尖,其他途径如经锁骨下动脉、经颈动脉、胸主动脉、腹主动脉、髂动脉、腋动脉等等也有少量病例报道。本年度多个研究显示,TAVR的多种路入途径都是可行的。
Arai T[4]分析了2011年1月至2014年12月 467例经股动脉、289例经升主动脉及42例经心尖TAVR患者的数据,发现经股动脉途径患者30天死亡率有低于经主动脉患者的趋势(5% vs. 9%; P = 0.057),而经升主动脉途径与经心尖途径30天死亡率无差异(9% vs.14%; P= 0.283)。该研究结论是,对于经股动脉不可行的病例,经升主动脉途径可作为经心尖途径的替代途径。
另外一个研究也得出类似的结论 [5]。Fiorina C研究显示,经腋下动脉途径和经升主动脉途径比,具有类似的手术成功率以、30天安全性以及一年的有效性[6]。
Biancari F采用倾向得分匹配的方法,对199对外科手术风险接近的患者进行对比,研究显示,经股动脉途径TAVR的短期及长期生存率均高于经心尖途径[7],这与既往一些研究结论是一致的。
Ciuca C研究显示,经心尖途径(N=142)与经锁骨下动脉途(N=60)径比,围手术期死亡率有增加的趋势 (8.4%vs. 1.7%, P = 0.06),虽然两组的1年及2年死亡率无差异。英国的TAVR注册研究 (N=3962)对各种TAVR入路途径也进行了比较,主要终点为2年生存率[9]。结果发现:经锁骨下动脉途径与经股动脉途径比,2年生存率无差异;而经心尖组及经主动脉途径与经股动脉途径组比,2年生存率均较低。
经颈动脉途径是TAVR另一种新途径。其优点包括:①路入途径短且笔直,输送系统易于控制,瓣膜位置容易调整,对于自膨胀瓣膜可实现回收;②血管表浅,容易分离、缝合;③血管较粗大,可进入较大鞘管[10]。较大样本的病例研究显示,该途径安全可行[11]。
新近,一种经股静脉到下腔静脉再到腹主动脉的路径,也成为TAVR手术新的路入途径。初步小样本的研究显示,该方法是安全可行的[12]。
综上,目前TAVR的入路处于多种方法存在、百花齐放的局面。总体上来看,经锁骨下动脉途径生存率与经股动脉接近,这两者为优选途径。而经升主动脉途径与经心尖途径生存率接近,劣于前面两种途径,应在前两种无法实施时选用。经颈动脉途径和经下腔静脉-主动脉途径也可能是较好的手术入路,但需要更多证据。
极简式TAVR
传统的TAVR是在杂交手术室、全麻、食道超声、外科医师甚至体外循环备台的情况下实施,这样可以最大程度保障手术的安全性。随着技术的改进及经验的积累,TAVR已经变得越来越安全。一些学者认为,TAVR可以像经皮冠脉介入(PCI)那样方式实施,于是极简式(minimalist approach)TAVR的概念被提出。
2014年,BabaliarosV 等首先提出极简式TAVR的概念[13]。手术是在传统的导管室下进行,采用局部麻醉加轻微的镇静(在手术医师的要求下,由护士给药而非麻醉师短暂的给予芬太尼+咪唑酮),由经胸心脏超声监测,通过股动脉路入,皮下穿刺、血管缝合器缝合,给予尿套而不是导尿管,无需外科医师在场备台或协助。这种手术方式把传统繁琐、复杂的TAVR手术方式大大简化,甚至无需专业的麻醉医师上台。
Babaliaros V [13]研究共纳入142例患者,70例患者实施极简式的TAVR,70例患者实施传统的TAVR,两组的STS评分无差异(10.6 ± 4.3 vs.11.4 ± 5.8; p = 0.35)。极简式组所有患者手术均成功,1例患者术中转为气管插管,而传统组3例患者发生操作相关性死亡。极简式组手术时间、住在ICU时间、住院时间以及费用大大低于传统手术组。两组30天死亡率、脑卒中以及中期随访的死亡率无差异。该研究提示极简式TAVR安全有效性不劣于传统TAVR,且能降低手术时间、住院时间以及相关费用。Jensen HA的研究也证实极简式TAVR的可行性及优点[14]。
Jabbar A研究证实,局麻下的TAVR的安全性不劣于全麻,且能降低手术时间、住院时间以及相关费用,为极简式TAVR可行性也提供了证据[15]。
大型注册研究AQUA研究纳入17 919台TAVR手术,分析有无外科医生在场(on-site)对手术结局的影响。结果发现虽然无外科医生在场的病例组年龄较大,估测的手术的风险较高,但是其住院期间死亡率与有外科医师在场的TAVR组无差异。该研究证实无外科医师在场的TAVR是安全可行的,为极简式的TAVR提供了有力证据。目前,由于简单、安全、有效、费用低,极简式TAVR已被越来越多的中心所接受[16]。
瓣膜退化,引发关注
Sawaya F研究显示,第一代的SAPIEN瓣膜,持久性良好,随访 5年内,410例患者瓣膜均未发现明显退化[17]。然而,欧洲血运重建大会(EuroPCR) 2016年会上发布的一项有关早期TAVR瓣膜长期耐久性的报告显示,第一代TAVR瓣膜半数会在8年内退化[18]。
该研究评估了704名患者,平均年龄82岁,在2002年4月至2011年5月之间接受TAVR,随访时间5年以上。排除死亡人数、30天内TAVR置入失败、瓣中瓣治疗等患者后共有378名患者接受为期10年的随访,进行超声心动图重复检测。随访显示,100例存活五年以上的患者的瓣膜出现退化,这里的退化定义为与心内膜炎无关的30天后出现的中/重度瓣膜反流或主动脉狭窄(平均梯度≥ 20 mmHg)。退化瓣膜大约2/3表现为瓣膜反流,1/3为瓣膜狭窄,极少数病例同时存在反流和狭窄,绝大多数瓣膜退化发生在术后5~7年。瓣膜8年退化的Kaplan-Meier估计值接近50%。
该研究给我们带来重要的启示,目前条件下,应该警惕把TAVR应用到太年轻、预期寿命较长的患者。虽然,TAVR瓣膜出现退化后,可以再次使用瓣中瓣技术,再次TVAR植入瓣膜,但是两个介入生物瓣膜的预期寿命可能就15-20年。并且,如果患者本来植入的瓣膜型号较小,采用瓣中瓣的方法也不一定合适。一般来说,生物瓣的寿命可达15年。TAVR的瓣膜采用的是和外科生物瓣相同的材料,理论上其寿命应该和外科生物瓣相同。这个研究结果显示,TAVR的寿命可能要比外科生物瓣短,有些令人意外。
笔者认为其原因可能原因包括:①手术因素:TAVR手术时装载压缩瓣膜或者球囊扩张时损伤到生物瓣膜;②血流动力学因素:由于瓣膜缝合方式不同或支架展开不全,TAVR瓣膜的血流动力学效应和外科生物瓣不同;③病人因素:TAVR的患者年龄更高、病情更危重、合并症更多,植入生物瓣膜本身就容易钙化。
目前全国约有10多个省市、20余家医院共完成600余例TAVR手术。其中,北京阜外心血管病医院、浙江大学附属第二医院、四川华西医院、复旦大学附属中山医院这四家医院手术量较大,是比较成熟的TAVR中心。大多数的病例使用的国产瓣膜,国产瓣膜成为主流。杭州启明的Venus-A瓣膜、上海微创的VitaFlow、苏州杰成的J-Valve均已完成临床试验的患者入组,初步统计结果显示着3个瓣膜安全有效,这3个产品均有望在明年获得中国食品药品管理局(SFDA)批准上市。国产瓣膜的预计价格要明显低于国外瓣膜。
我国估计有数百万的主动脉瓣疾病患者,TAVR是一种前景广阔的革命性新技术。国产瓣膜一旦获批上市,我国TAVR病例数将出现指数级增长,使得广大的患者获益。国产瓣膜也很可能是未来我国TAVR的主流器械。
目前,TAVR正向精细化发展。回顾本年的文献,可发现许多文献都是针对TAVR的技术细节或者特定的临床问题进行深入研究,并取得一定进展。由于研究较多,不一一罗列,下面介绍几个比较主要的研究。
波兰注册研究显示,TAVR术后单用阿司匹林是可行的,可减少血管并发症[19]。TVT 注册研究显示,TAVR术后植入永久起搏器比较常见,植入永久起搏器者1年死亡率及心衰发生率相对较较高[20]。Condado JF发表研究显示,TAVR术前行颈动脉血管评估并不能降低脑卒中发生率[21]。Gaglia MA Jr的研究显示,女性患者接受TAVR术血管并发症发生率较高,但是30天死亡率及1年死亡率更低[22]。
Regueiro A对20 006例TAVR资料分析显示,感染性心内膜炎发生率为1.1%/人年,感染性心内膜炎中期发生时间为5.3月(四分位时间,1.5-13.4月),年轻、男性、糖尿病病史、中度至重度瓣周漏者容易发生染性心内膜炎[23]。
主动脉瓣狭窄可以并发不明原因的消化道出血,这被称之为Heyde 综合征,血管性假血友病因子多聚体(VWF multimers )降低是其中一个重要机制[24]。Van Belle E研究[25]发现,TAVR可以纠正VWF multimers 的异常降低,但是残存的瓣周漏影响了VWF multimers 的恢复,残留有瓣周漏患者的VWF multimers 水平能较低;VWF multimers 水平可以非常准确的预测瓣周漏,并且与1年死亡率明显相关。
CLEAN-TAVI 研究探讨了脑血栓保护装置对TAVR 手术脑卒中的保护作用,共入选100例患者,随机分为器械保护组和无保护组,结果显示保护组颅脑损害新发的病变个数以及病变的体积均少于无保护组,但由于样本量较少,两组的脑血管事件上无差异[26]。该研究显示血栓保护装置对TAVR术中脑血管事件的预防可能是有效的。
原始出处:
[1] Leon MB, Smith CR, Mack MJ, et al; PARTNER 2 Investigators. Transcatheter or Surgical Aortic-Valve Replacement in Intermediate-Risk Patients. N Engl J Med, 2016,374(17):1609-20.
[2] Thourani VH, Kodali S, Makkar RR,et al.Transcatheter aortic valve replacement versus surgical valve replacement in intermediate-risk patients: a propensity score analysis,Lancet, 2016;387(10034):2218-25.
[3] Reardon MJ, Kleiman NS, Adams DH, et al. Outcomes in the Randomized CoreValve US Pivotal High Risk Trial in Patients With a Society of Thoracic Surgeons Risk Score of 7% or Less. JAMA Cardiol, 2016,1(8):945-949.
[4] Arai T, Romano M, Lefèvre T, et al. Direct Comparison of Feasibility and Safety of Transfemoral Versus Transaortic Versus Transapical Transcatheter Aortic Valve Replacement. JACC Cardiovasc Interv, 2016,9(22):2320-2325.
[5] Bapat V, Frank D, Cocchieri R, et al. Transcatheter Aortic Valve Replacement Using Transaortic Access: Experience From the Multicenter, Multinational, Prospective ROUTE Registry. JACC Cardiovasc Interv, 2016,9(17):1815-22.
[6] Fiorina C, Bruschi G, Testa L, Trans-axillary versus trans-aortic approach for transcatheter aortic valve implantation with corevalve revalving system: insights from multicentre experience. J Cardiovasc Surg (Torino). 2016 Oct 4. [Epub ahead of print]
[7] Biancari F, Rosato S2 D'Errigo P,et al. Immediate and Intermediate Outcome After Transapical Versus Transfemoral Transcatheter Aortic Valve Replacement. Am J Cardiol, 2016,117(2):245-51.
[8] Ciuca C, Tarantini G, Latib A, et al.Trans-subclavian versus transapical access for transcatheter aortic valve implantation: A multicenter study.Catheter Cardiovasc Interv,2016,87(2):332-8.
[9] Fröhlich GM, Baxter PD, Malkin CJ,et al; National Institute for Cardiovascular Outcomes Research.Comparative survival after transapical, direct aortic, and subclavian transcatheter aortic valve implantation (data from the UK TAVI registry).
Am J Cardiol,2015 ,116(10):1555-9.
[10] 潘文志, 周达新, 张蕾, 等. 经颈动脉途径行经导管主动脉瓣置入术一例 [J]. 中华心血管病杂志,2016,44( 4 ): 348-349.
[11] Mylotte D, Sudre A, Teiger E,et al.Transcarotid Transcatheter Aortic Valve Replacement: Feasibility and Safety. JACC Cardiovasc Interv, 2016,9(5):472-80.
[12] Greenbaum AB, Babaliaros VC, Chen MY, et al. Transcaval access and closure for transcatheter aortic valve replacement: a prospective investigation. J Am Coll Cardiol. 2016;Epub ahead of print.
[13] Babaliaros V, Devireddy C, Lerakis S, et al. Comparison of transfemoral transcatheter aortic valve replacement performed in the catheterization laboratory (minimalist approach) versus hybrid operating room (standard approach): outcomes and cost analysis.JACC Cardiovasc Interv, 2014,7(8):898-904.
[14] Jensen HA, Condado JF, Devireddy Minimalist transcatheter aortic valve replacement: The new standard for surgeons and cardiologists using transfemoral access?J Thorac Cardiovasc Surg, 2015,50(4):833-9.
[15] Jabbar A, Khurana A, Mohammed A, et al. Local Versus General Anesthesia in Transcatheter Aortic Valve Replacement.Am J Cardiol,.2016,118(11):1712-1716.
[16] Eggebrecht H, Bestehorn M, Haude M, et al.Outcomes of transfemoral transcatheter aortic valve implantation at hospitals with and without on-site cardiac surgery department: insights from the prospective German aortic valve replacement quality assurance registry (AQUA) in 17 919 patients.Eur Heart J, 2016,37(28):2240-8.
[17] Sawaya FJ, Lefèvre T, Spaziano M,et al.Transfemoral Transcatheter Aortic Valve Implantation: How Minimalistic Can We Become? J Interv Cardiol, 2016,29(6):628-631.
[18] Sawaya F, Kappetein AP, Wisser W, et al. Five-year haemodynamic outcomes of the first-generation SAPIEN balloon-expandable transcatheter heart valve. EuroIntervention, 2016,12(6):775-82.
[19]http://www.pcronline.com/News/Press-Releases/EuroPCR-2016-Half-of-transcatheter-heart-valves-show-degeneration-within-10-years-of-TAVI
[20] Czerwińska-Jelonkiewicz K, Zembala M, Dąbrowski M, et al. Can TAVI patients receive aspirin monotherapy as patients after surgical aortic bioprosthesis implantation? Data from the Polish Registry - POL-TAVI. Int J Cardiol. 2016 Nov 9. pii: S0167-5273(16)33551-3. doi: 10.1016/j.ijcard.2016.11.095. [Epub ahead of print]
[21] Fadahunsi OO, Olowoyeye A, Ukaigwe A, et al. Incidence, Predictors, and Outcomes of Permanent Pacemaker Implantation Following Transcatheter Aortic Valve Replacement: Analysis From the U.S. Society of Thoracic Surgeons/American College of Cardiology TVT Registry. JACC Cardiovasc Interv, 2016,9(21):2189-2199.
[22] Condado JF, Jensen HA, Maini A, et al. Should We Perform Carotid Doppler Screening Before Surgical or Transcatheter Aortic Valve Replacement? Ann Thorac Surg. 2016 Oct 4. pii: S0003-4975(16)30792-5. doi: 10.1016/j.athoracsur.2016.06.076. [Epub ahead of print]
[23] Gaglia MA Jr, Lipinski MJ, Torguson R,et al .Comparison in Men Versus Women of Co-morbidities, Complications, and Outcomes After Transcatheter Aortic Valve Implantation for Severe Aortic Stenosis. Am J Cardiol, 2016, 118(11):1692-1697.
[24] Regueiro A, Linke A, Latib A,et al. Association Between Transcatheter Aortic Valve Replacement and Subsequent Infective Endocarditis and In-Hospital Death. JAMA, 2016,316(10):1083-92.
[25] Spangenberg T, Budde U, Schewel D, et al. Treatment of acquired von Willebrand syndrome in aortic stenosis with transcatheter aortic valve replacement. JACC Cardiovasc Interv, 2015 ,8(5):692-700.
[26] Van Belle E, Rauch A,, Vincent F,et al. Von Willebrand Factor Multimers during Transcatheter Aortic-Valve Replacement. N Engl J Med, 2016,375(4):335-44.
[27] Haussig S1, Mangner N1, Dwyer MG,et al. Effect of a Cerebral Protection Device on Brain Lesions Following Transcatheter Aortic Valve Implantation in Patients With Severe Aortic Stenosis: The CLEAN-TAVI Randomized Clinical Trial. JAMA, 2016,316(6):592-601.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#置换#
36
#精细化#
31
#主动脉瓣#
0
#主动脉#
29
#经导管#
27
#经导管主动脉瓣置换#
31
#葛均波院士#
28