JACC:经导管主动脉瓣膜置换术临床获益持续可达三年
2016-04-09 MedSci MedSci原创
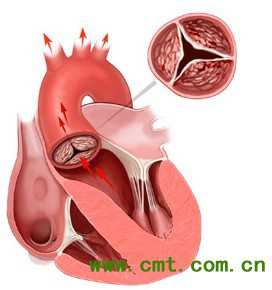
背景:手术风险增加的严重主动脉瓣狭窄患者手术,与手术相比,经导管主动脉瓣置换(TAVR)与患者2年生存率改善相关。目的:研究者旨在确定临床获益的持续时间。方法:研究者将由多学科中心组确认的手术风险增加的严重主动脉瓣狭窄患者,按照1:1比例随机分为TAVR组或开放手术瓣膜置换术(SAVR)组。按照程序获得这些患者3年的临床和超声心动图的结果。结果:共招募美国45个中心的797例患者,750例患者纳入
背景:手术风险增加的严重主动脉瓣狭窄患者手术,与手术相比,经导管主动脉瓣置换(TAVR)与患者2年生存率改善相关。
目的:研究者旨在确定临床获益的持续时间。
方法:研究者将由多学科中心组确认的手术风险增加的严重主动脉瓣狭窄患者,按照1:1比例随机分为TAVR组或开放手术瓣膜置换术(SAVR)组。按照程序获得这些患者3年的临床和超声心动图的结果。
结果:共招募美国45个中心的797例患者,750例患者纳入研究。TAVR组患者三年全因死亡或卒中发生率显著降低(37.3% vs 46.7% SAVR;P = 0.006)。与SAVR组相比,TAVR组不良临床预后也下降,包括全因死亡率(32.9% vs 39.1%;P = 0.068),所有卒中(12.6% vs 19%;P = 0.034),和主要不良心脑血管事件(40.2%和47.9%;P = 0.025)。尽管TAVR组患者存在中度或重度主动脉瓣反流,但3年主动脉瓣血流动力学研究中,TAVR组优于SAVR组(平均主动脉瓣梯度,7.62±3.57mmHg vs 11.40±6.81 mm Hg,P<0.001)。两组均无瓣膜血栓形成的临床证据。
结论:手术风险增加的严重主动脉瓣狭窄患者TAVR治疗后的3年临床预后优于手术组。两组间瓣膜结构的变化没有差异,但TAVR组主动脉瓣血流动力结果更有利。
原文出处:
Deeb GM, Reardon MJ, et al. Three-Year Outcomes in High-Risk Patients Who Underwent Surgical or Transcatheter Aortic Valve Replacement. J Am Coll Cardiol. 2016 Mar 22.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#经导管主动脉瓣膜置换术#
36
#置换#
19
#临床获益#
31
#JACC#
27
#瓣膜置换术#
39
文章不错
80
值得学习
114
#ACC#
20
#主动脉瓣#
17
#主动脉#
18