Oncogene:肿瘤微环境通过外泌体向癌细胞传授生存技巧
2016-11-15 佚名 生物谷
-根据国际学术期刊Cancer Research上的一项研究,胰腺癌是导致癌症相关死亡的第三大癌症类型,预计到2030年将上升为第二。胰腺癌病人的5年生存率只有8%,是唯一一个生存率仅为个位数的主要癌症类型。虽然胰腺癌病人的死亡率很高,但是对胰腺癌的研究和资助仍然不足,目前通过FDA审批用以治疗这种疾病的方法仍然很少。 由于美国圣母诺丹特

根据国际学术期刊Oncogene上的一项研究,胰腺癌是导致癌症相关死亡的第三大癌症类型,预计到2030年将上升为第二。胰腺癌病人的5年生存率只有8%,是唯一一个生存率仅为个位数的主要癌症类型。虽然胰腺癌病人的死亡率很高,但是对胰腺癌的研究和资助仍然不足,目前通过FDA审批用以治疗这种疾病的方法仍然很少。
由于美国圣母诺丹特大学Dr. Reginald Hill领导的研究团队取得了一项最新研究进展,受胰腺癌折磨的病人未来将有更好的治疗选择。Hill的研究重点在已经通过FDA 审批的一些药物,他们希望通过研究找出药物对胰腺癌病人不起作用的原因。
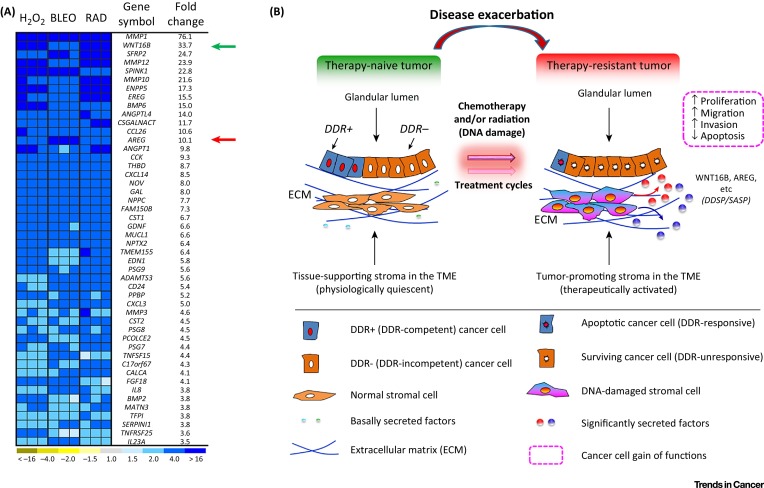
“胰腺肿瘤由大约10%的癌细胞和90%的支持细胞组成。支持细胞掌握了如何在化疗中存活下来的技巧,”Hill这样说道。“在化疗过程中,支持细胞会释放出包裹着遗传物质的外泌体,教会癌细胞如何存活,导致肿瘤发生化疗抵抗。”
发表在NEJM上的一项研究已经发现大多数胰腺癌病例会抵抗化疗,并且对那些在其它类型癌症中发挥治疗作用的药物不产生应答。
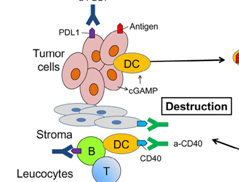
大多数新研究都聚焦在如何摧毁支持细胞,但是那些研究发现当支持细胞受到攻击,病人的癌症病情会进一步发展。“这就像在癌细胞周围的区域捅出一些洞,这样癌细胞就可以向外扩散。”
Hill主要进行阻断外泌体释放的研究,阻止支持细胞将信息传递给癌细胞,这样就能增加化疗的效果。这项最近发表的研究表明,使用无毒性的外泌体阻断剂结合标准化疗方法能够增强对胰腺癌和其他一些癌症的治疗效果。
为许多没有理想治疗选择的胰腺癌病人找到有效的治疗方法是Hill继续研究的动力。这项最新发现将为胰腺癌病人带来了新的希望。
原始出处
Richards KE, Zeleniak AE, Fishel ML, Wu J, Littlepage LE, Hill R. Cancer-associated fibroblast exosomes regulate survival and proliferation of pancreatic cancer cells. Oncogene. 2016 Sep 26. doi: 10.1038/onc.2016.353
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Gene#
31
还是要看原文 多深层理解 找到自己想要的
59
讲得好,学习了
78
#癌细胞#
31
#Oncogene#
32