BMC Ophthalmol :泪腺脱出程度与甲状腺相关眼病临床特征相关性的回顾性观察
2022-03-04 从医路漫漫 MedSci原创
甲状腺相关眼病(TAO)是Graves病最常见的甲状腺外表现,25-50%的患者有此病。先前的研究表明,65-85%的TAO患者有泪腺受累,这会导致泪液分泌减少。
背景:甲状腺相关眼病(TAO)是Graves病最常见的甲状腺外表现,25-50%的患者有此病。先前的研究表明,65-85%的TAO患者有泪腺受累,这会导致泪液分泌减少。患者通常会抱怨泪水过多、畏光、沙粒、异物感和干眼症的其他症状。几项磁共振成像(MRI)和计算机断层扫描(CT)研究表明,TAO患者的泪腺体积明显大于健康对照组。临床上,TAO患者不仅泪腺增大,而且脱出眶外,但目前对TAO患者泪腺脱垂(LGP)的相关因素知之甚少。因此,本研究的目的是寻找一种简便的定量MRI参数来衡量LGP的程度,并作为TAO活动性的良好指标。关于甲状腺相关眼病(TAO)患者泪腺脱垂(LGP)相关因素的研究较少。本研究旨在探讨磁共振成像(MRI)上LGP的相关因素及其与TAO活动性的关系。
方法:对36例(72对眼睛)非活动期(43对眼睛,临床活动评分<3分)或活动期(29对眼睛,CAS≥为3分)患者进行回顾性研究。所有患者均接受眼科检查和眼眶磁共振成像。测量LGP、眼球突出的严重程度和眼外肌(EOM)体积。对LGP及相关因素进行相关分析和线性回归分析。通过受试者工作特征曲线分析,评价LGP对TAO活动性的判别价值。
结果:活动期TAO组的平均LGP明显高于非活动期TAO组(P<0.001)。LGP严重程度与颈总动脉(r=0.51P<0.001)、前凸(r=0.72,P<0.001)、上直肌[r=0.49,P<0.001]、下直肌[r=0.47,P<0.001]、外直肌[r=0.59,P<0.001]、内直肌[r=0.62,P<0.001]、上斜肌[r=0.48,P<0.001]、。各组间差异有统计学意义(r=0.59P<0.001)。受试者操作特征曲线分析显示,LGP13.65 mm(曲线下面积为0.824;敏感性为79.3%;特异性为81.4%)是区分活动性和非活动性TAO的临界值。
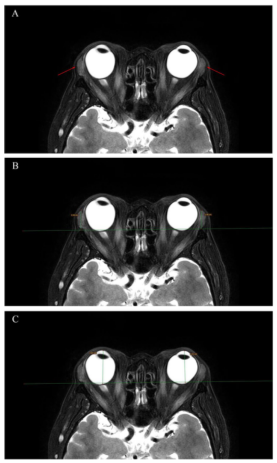
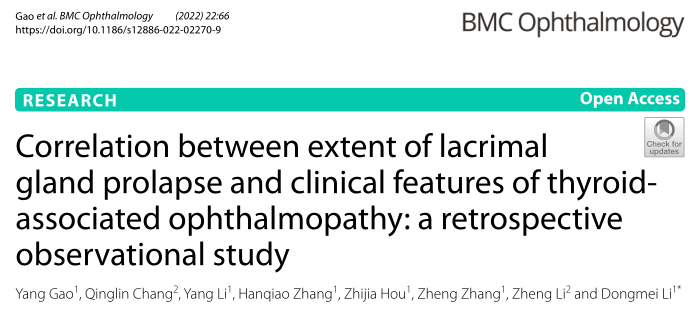
图1甲状腺相关眼病患者的轴位3毫米厚T2加权脂肪抑制图像。(A)中的箭头显示双侧泪腺脱垂。(B)泪腺脱垂,以泪腺顶部至颧间线的垂直距离量度,右侧为15.1毫米,左侧为14.6毫米。(C)眼球突出是指角膜顶部到颧间线的垂直距离。
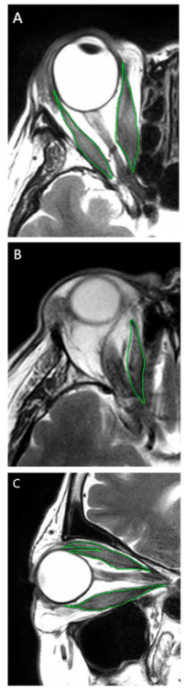
图2在T2加权磁共振成像扫描上测量眼外肌横截面积。(A)内直肌和外直肌的面积由轴位图像获得。(B)上斜肌面积由轴位图像获得。(C)上直肌复合体和下直肌的面积由矢状位图像获得。
表1 活动性与非活动性甲状腺相关眼病的人口学和定量测量比较
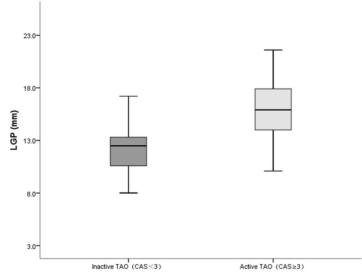
图3比较活动期TAO组和非活动期TAO组泪腺下垂程度的曲线图。曲线图和条形图表示平均值和标准差。活动组的平均LGP明显大于非活动组(P<0.001)。CAS,临床活动评分;LGP,泪腺脱垂;TAO,甲状腺相关眼病
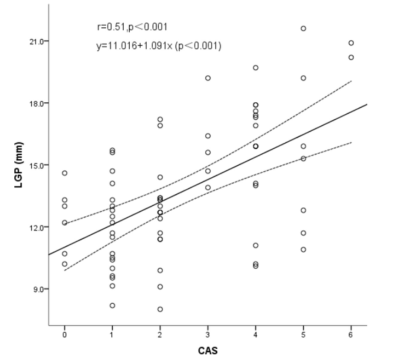
图4泪腺脱垂程度与临床活动评分呈显著正相关(r=0.51P<0.001),直线回归方程为:Y=11.016+1.091X(P<0.001)。LGP,泪腺脱垂;CAS,临床活动评分

图5泪腺脱垂程度与突出量呈显著正相关(r=0.72P<0.001)。直线回归方程为:Y=2.215+0.654x(P<0.001)。LGP,泪腺脱垂
结论:眼眶磁共振图像的LGP测量值与CAS、眼球突出度和EOM体积呈正相关。LGP的范围似乎是TAO患者疾病活动性的一个很好的指标。
原文出处:Gao Y, Chang Q, Li Y,et al.Correlation between extent of lacrimal gland prolapse and clinical features of thyroid-associated ophthalmopathy: a retrospective observational study.BMC Ophthalmol 2022 Feb 10;22(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#相关性#
34
#BMC#
34
#临床特征#
38
#眼病#
41
#THA#
30