Circulation:抑制PI3Kγ可预防蒽环类药物的心毒性,同时可减缓肿瘤生长
2018-08-17 MedSci MedSci原创
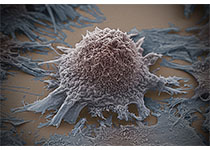
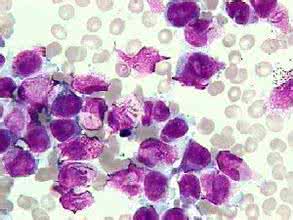
蒽环类药物,如阿霉素(DOX),是有效抗癌(实体肿瘤和血液恶性肿瘤)药物。但是,其临床应用受到心脏毒性的限制。现有研究人员对磷酸肌醇3激酶γ(PI3Kγ)在DOX诱导的心脏毒性中的作用,以及PI3Kγ抑制剂潜在的心脏保护和抗癌作用进行研究。用DOX长期处理表达PI3Kγ或接受PI3Kγ选择性抑制剂处的小鼠。用心脏超声分析心功能,并评估整个心脏或分离的心肌的DOX介导的信号。在小鼠乳腺癌模型中评估P
用DOX长期处理表达PI3Kγ或接受PI3Kγ选择性抑制剂处的小鼠。用心脏超声分析心功能,并评估整个心脏或分离的心肌的DOX介导的信号。在小鼠乳腺癌模型中评估PI3Kγ抑制剂的心脏保护和抗肿瘤效应。
PI3Kγ激酶抑制的小鼠在长期小剂量DOX处理后心脏功能未受损,提示其可抵抗DOX诱导的心毒性。PI3Kγ抑制剂的有利效应主要是通过增强DOX破坏的线粒体自噬清除来实现的。与之相一致,药物或遗传阻断体内的自噬清除即可破坏PI3Kγ激酶抑制小鼠对DOX心毒性的抵抗力。机制上,在DOX处理的心脏中,Toll样受体9的下游,PI3Kγ被损伤的细胞器所释放的和自噬体所吞噬的线粒体DNA激活。自噬体PI3Kγ/Akt/mTor/UIK1信号通过不良适应反馈抑制自噬。在乳腺癌模型中阻断PI3Kγ可预防DOX诱导的心功能不全,同时,通过释放抗癌免疫增强DOX的抗肿瘤活性。
在抗癌治疗中,封闭PI3Kγ或可发挥双重治疗效应,即预防蒽环类药物的心毒性和减缓肿瘤生长。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PI3K#
30
#蒽环类药物#
37
#蒽环类#
46
不错耶,学习了
43
学习学习谢谢
62
学习
52