Science:白细胞介素-22结合蛋白参与炎症性肠病的发生发展
2016-10-23 xing.T MedSci原创
这些研究结果表明,抗TNF-α疗法可能至少部分是通过抑制IL-22BP,该研究指明一个更具体的潜在的治疗IBD的靶点。
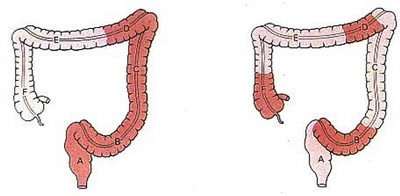
肠道炎症可损害粘膜愈合,从而建立了一个恶性循环,导致慢性炎症性肠病(IBD)。然而,驱动慢性炎症的信号网络仍不清楚。最近,顶级杂志《Science》上发表文章旨在探究白细胞介素-22(IL-22) 结合蛋白与IBD的关系。 研究者发现从IBD患者分离出的CD4+T细胞高表达白细胞介素-22结合蛋白(IL-22BP),IL-22BP作为组织保护性细胞因子IL-22的内源性抑制剂。利用小鼠模型,研究者发现IBD的发展需要T细胞合成分泌的IL-22BP。最后,从IBD患者中分离出的肠道CD4 + T细胞对目前最有效的IBD治疗方式-抗肿瘤坏死因子–α抗体(抗TNF–α治疗)有效果,并能够有效的降低IL-22BP表达量,但不影响IL-22的表达。 这些研究结果表明,抗TNF-α疗法可能至少部分是通过抑制IL-22BP,该研究指明一个更具体的潜在的治疗IBD的靶点。 原始出处: Penelope Pelczar, et al. A pathogenic role for T cell–derived IL-22BP in inflammatory bowel disease. 2016.Scie
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#白细胞介素-2#
45
#发生发展#
35
#SCIE#
31
#炎症性#
23
#白细胞介素#
52