Inflamm Bowel Dis:内镜下黏膜愈合是炎症性肠病的有利预测因素
2016-07-07 Mechront 译 MedSci原创
根据近期一项荟萃分析的结果,对于炎症性肠病患者,内镜下黏膜愈合是有利的临床结局重要预测因素,包括更少的手术、住院治疗和长期临床缓解。“溃疡性结肠炎(UC)和克罗恩病(CD)是主要的肠道粘膜炎症和溃疡性疾病,内镜下黏膜愈合(MH)作为一个关键的替代终点已经上升到突出地位。”来自密歇根大学的Ann Arbor研究人员写道。研究人员回顾了所有发表的有关队列研究和随机对照试验,评估IBD治疗的MH区间,随
根据近期一项荟萃分析的结果,对于炎症性肠病患者,内镜下黏膜愈合是有利的临床结局重要预测因素,包括更少的手术、住院治疗和长期临床缓解。
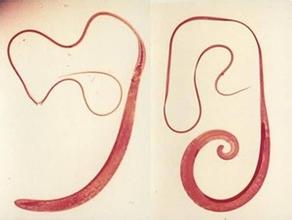
“溃疡性结肠炎(UC)和克罗恩病(CD)是主要的肠道粘膜炎症和溃疡性疾病,内镜下黏膜愈合(MH)作为一个关键的替代终点已经上升到突出地位。”来自密歇根大学的Ann Arbor研究人员写道。
研究人员回顾了所有发表的有关队列研究和随机对照试验,评估IBD治疗的MH区间,随访愈合和不愈合的患者,并记录手术、住院和临床缓解等相关数据。最终包括19项研究(n = 2,256)进行荟萃分析。
汇总分析显示,UC和CD患者与不愈合的患者相比,MH与更少的腹部大手术有关(RR = 0.34; 95% CI, 0.26-0.46),更少的住院有关(RR = 0.58; 95% CI, 0.42-0.78),还与缓解率的增加相关(RR = 1.84; 95% CI, 1.43-2.36)。分开分析CD和UC患者,MH能预测更少的手术和缓解率的增加,但是对于CD和UC患者住院情况方面,尚缺乏比较证据。
与不愈合的患者相比,完全和部分MH对结局的预测更好,完全 vs.部分MH,在手术预测方面没有显著差异,不过完全MH预测无皮质类固醇缓解率上更好(RR = 1.71; 95% CI, 1.24-2.34)。Meta回归分析显示,完全和部分MH的缓解预测能力与随访时间密切相关。
分析结果表明,对于炎症性肠病患者,内镜下黏膜愈合是有利的临床结局重要预测因素,包括更少的手术、住院治疗和长期临床缓解。
原始出处:
Reinink AR, et al. Inflamm Bowel Dis. 2016;doi:10.1097/MIB.0000000000000816.
Mucosal healing strongly associated with positive clinical outcomes in IBD.Healio.July 6, 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#黏膜愈合#
42
#LAM#
29
#Dis#
23
#Bow#
22
#内镜#
19
#预测因素#
25
#NFL#
18
#bowel#
20
#黏膜#
30
#炎症性#
23