Nat Commun:乙肝病毒导致肝癌的免疫逃逸机制研究新进展
2018-04-01 佚名 中科大生科院
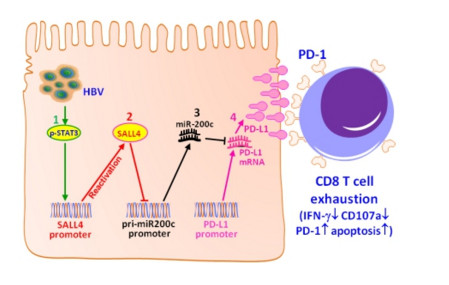
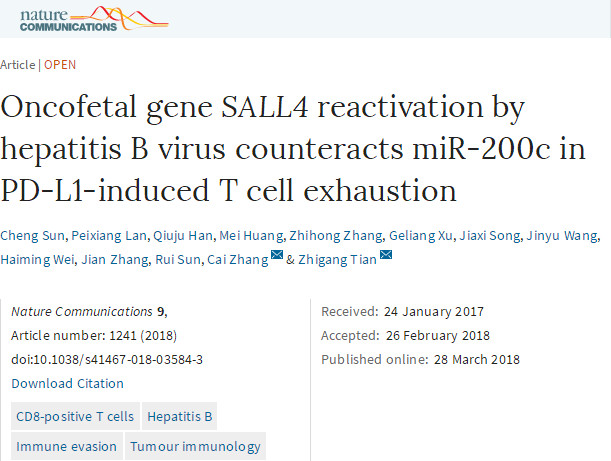
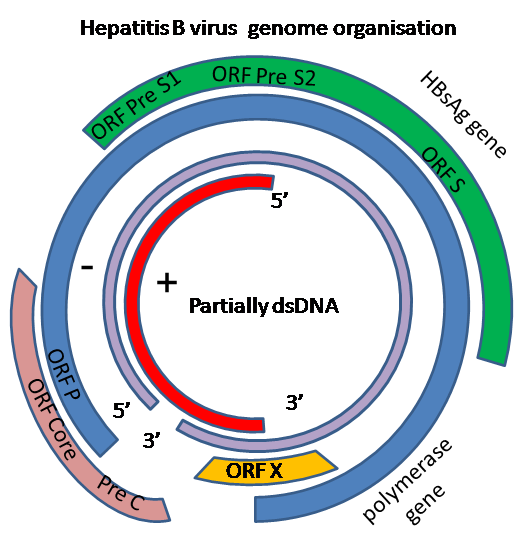
近日,《Nature Communications》杂志在线发表了中国科学技术大学与山东大学联合攻关的研究论文“Oncofetal gene SALL4 reactivation by hepatitis B virus counteracts miR-200c in PD-L1-induced T cell exhaustion”,该项研究成果揭示了乙肝病毒感染导致机体T淋巴细胞免疫耗竭的新机制
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Nat#
32
#机制研究#
23
#COMMUN#
24
#免疫逃逸机制#
44
学习学习.理论进步了
62
学习了.谢谢作者分享!
61