Cell:张旭发现FGF13调节神经极化和迁移过程
2012-06-25 bo 生物谷
6月22日,Cell杂志报道:上海神经科学研究所张旭研究组发现成纤维细胞生长因子13在神经细胞中作为微管稳定蛋白发挥重要调节功能。 分泌性成纤维细胞生长因子(FGFs)和其受体在神经系统发育的早期阶段发挥调节功能。 FGF13,是FGF家族的非分泌性蛋白质。它在神经发展过程中表达于大脑皮质神经元,是综合征性及非特异性X染色体连锁性智障(XLMR)的候选基因。然而,其在神经发育过程中的功能尚不清楚

6月22日,Cell杂志报道:上海神经科学研究所张旭研究组发现成纤维细胞生长因子13在神经细胞中作为微管稳定蛋白发挥重要调节功能。
分泌性成纤维细胞生长因子(FGFs)和其受体在神经系统发育的早期阶段发挥调节功能。 FGF13,是FGF家族的非分泌性蛋白质。它在神经发展过程中表达于大脑皮质神经元,是综合征性及非特异性X染色体连锁性智障(XLMR)的候选基因。然而,其在神经发育过程中的功能尚不清楚。
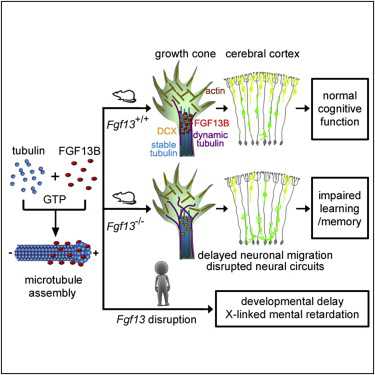
本研究表明,FGF13在细胞内作为轴突必须的微管稳定蛋白并在大脑皮层神经细胞迁移中起着引导的重要作用。 FGF13富集于轴突生长锥,并直接与微管相互作用。此外,FGF13聚合微管蛋白并稳定微管。 敲除FGF13基因可损害神经元极化并增加轴突的分支化和引导生长作用。 FGF13的基因缺失可导致小鼠大脑皮层和海马的神经细胞迁移缺陷。 FGF13缺陷小鼠也表现出学习和记忆能力的减退。这与XLMR患者的智力残疾是想对应的。
总之,本研究揭示了FGF13在神经细胞极化和迁移中的重要作用,为XLMR等相关疾病的进一步研究带来新的重要启示。

doi:10.1016/j.cell.2011.10.017
PMC:
PMID:
Fibroblast Growth Factor 13 Is a Microtubule-Stabilizing Protein Regulating Neuronal Polarization and Migration
Qing-Feng Wu, Liu Yang, Shuai Li, Qiong Wang, Xiao-Bin Yuan, Xiang Gao,Xu Zhang
Secretory fibroblast growth factors (FGFs) and their receptors are known for their regulatory function in the early stages of neural development. FGF13, a nonsecretory protein of the FGF family, is expressed in cerebral cortical neurons during development and is a candidate gene for syndromal and nonspecific forms of X-chromosome-linked mental retardation (XLMR). However, its function during development remains unclear. We show that FGF13 acts intracellularly as a microtubule-stabilizing protein required for axon and leading process development and neuronal migration in the cerebral cortex. FGF13 is enriched in axonal growth cones and interacts directly with microtubules. Furthermore, FGF13 polymerizes tubulins and stabilizes microtubules. The loss of FGF13 impairs neuronal polarization and increases the branching of axons and leading processes. Genetic deletion of FGF13 in mice results in neuronal migration defects in both the neocortex and the hippocampus. FGF13-deficient mice also exhibit weakened learning and memory, which is correlated to XLMR patients' intellectual disability.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Cell#
26
#迁移#
23
#CEL#
17
#FGF1#
36