盘点:子宫内膜异位症近期重要研究进展一览
2017-09-03 MedSci MedSci原创
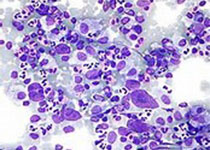
子宫内膜异位症是一种相对常见的疾病,指的是本应在子宫内生长的子宫内膜组织在子宫以外的其他组织上异常生长,通常病灶发生在腹腔和卵巢中。5-10%的育龄妇女受其影响,并导致了30-50%不育症的风险。这里梅斯小编整理了近期关于子宫内膜异位症的重要研究进展与大家一同分享。【1】子宫内膜异位的癌变风险如何研究人员通过外消旋测序(24例)或癌症-驱动靶向测序(3例)分析27例患者的深度浸润性子宫内膜异位
子宫内膜异位症是一种相对常见的疾病,指的是本应在子宫内生长的子宫内膜组织在子宫以外的其他组织上异常生长,通常病灶发生在腹腔和卵巢中。5-10%的育龄妇女受其影响,并导致了30-50%不育症的风险。这里梅斯小编整理了近期关于子宫内膜异位症的重要研究进展与大家一同分享。
【1】子宫内膜异位的癌变风险如何
研究人员通过外消旋测序(24例)或癌症-驱动靶向测序(3例)分析27例患者的深度浸润性子宫内膜异位病变。通过使用数字基因组方法在显微解剖上皮和基质中验证突变。通过用于反复激活KRAS突变的液滴数字聚合酶链反应(PCR)来分析另外12名患者的病变的上皮和基质组分。结果发现深部浸润性子宫内膜异位症的病变实际上与恶性转化的风险无关,其中存在体细胞癌症驱动突变。 39例深部浸润性病变中有10例(26%)携带有驱动突变;所有测试的体细胞突变似乎局限于子宫内膜异位病变的上皮部分。
【2】Elagolix治疗子宫内膜异位症的效果及安全性
子宫内膜异位症是一种慢性雌激素依赖性疾病,通常引起痛经(进行性加重)和盆腔疼痛 。Elagolix 是一种口服非肽类促性腺激素释放激素拮抗剂,在以往的研究中对雌激素产生部分至整体的抑制作用。近期,研究者进行了两个类似的为期六个月的双盲随机3期临床试验以评估低剂量组(150mg /每天一次)和高剂量组(200mg/每天两次)与安慰剂组对照的不同效应。结果在为期6个月的观察期内,无论是服用较高剂量还是较低剂量elagolix均能明显改善受试女性的痛经和非经期盆腔疼痛症状。两种剂量的elagolix与低雌激素的不良影响相关。表明elagolix在子宫内膜异位症治疗方面的疗效和安全性均已得到证实。
【3】子宫内膜异位的遗传学机制
最近由昆士兰大学的研究者们进行的一项有关子宫内膜异位疾病的大型遗传学研究结果揭示:5种基因的路边可能导致该疾病的发生。这项研究一共分析了20万女性的基因组构成,用于寻找引发子宫内膜异位的遗传学机制,这一发现将有助于未来相关治疗得开发。该研究验证了此前发现的11个与子宫内膜异位有关的基因,同时还发现了5个全新的遗传位点。除此之外,研究人员发现一些与雌二醇调节有关的基因似乎参与了子宫内膜异位的发生。这一发现能够给其他科学家们新的线索,以通过更多的研究揭示子宫内膜异位的遗传学机制。
【4】子宫内膜异位症与高胆固醇血症或高血压之间有何关系
以激素或慢性全身炎症环境改变为特征的子宫内膜异位症可能导致高胆固醇血症和高血压的发生风险增高。相反,由高血压引起的高胆固醇血症中低密度脂蛋白升高和慢性全身性炎症升高可能增加子宫内膜异位症的发生风险。近日,心血管权威杂志Hypertension上发表了一篇研究文章,研究人员在一项大型前瞻性队列研究中评估了腹腔镜确诊的子宫内膜异位症与高胆固醇血症和高血压之间的关系。其结果表明,经腹腔镜确诊的子宫内膜异位症与高胆固醇血症和高血压风险增加之间存在前瞻性的相关性。相反,高胆固醇血症和高血压也与较高的经腹腔镜确诊的子宫内膜异位症的发生风险之间存在前瞻性的相关性。
【5】子宫内膜异位症发病新机理
子宫内膜异位症被认为是这些恶性肿瘤的前驱病变。尽管如此,包括深度浸润的子宫内膜异位在内的绝大部分病变都不会发展为癌症。尽管研究人员发现,并发癌症的子宫内膜异位患者带有KRAS和PTEN等癌症相关的驱动突变,依然缺乏详尽的非癌症相关病变基因组分析。因此,在最近的一项报道中,Anglesio和他的同事们对非癌症相关病变诱发体细胞驱动突变进行了深入的研究。结果发现尽管没有任何病例表现出癌症或异常增生的迹象,大部分患者还是发生了体细胞突变(79%),其中5例带有PIK3CA, KRAS, 和ARID1A在内的癌症驱动突变。这项研究结果为子宫内膜异位症的发病机理提供了新的线索,一部分病人带有多个转移性病灶,一些病人的转移性病灶上发生了完全相同的突变。研究同时带来了一些新的问题,良性病变中已知癌症驱动突变作用如何,是否对带有致病突变的病变患者辅以靶向抗肿瘤药物治疗等。子宫内膜异位症病灶中体细胞突变的普遍存在,同样说明了无论是良性还是恶性病变,对患者病灶进行多基因全方位的筛查、诊断和分子分型都大有必要。
【6】TGF-β在腹膜子宫内膜异位症的病理生理中的作用
子宫内膜异位症的病因尚不能明确,不过越来越多的证据表明转化生长因子(TGF)-β发挥主要的作用。研究人员检索纳入了95项相关研究,汇总发现,与未患子宫内膜异位症的女性相比,子宫内膜异位症患者腹水、血清、子宫内膜异位灶和腹膜中TGF-β1的水平均增加,并且在TGF-β1沉默表达的小鼠中,子宫内膜异位损伤性生长较野生型对照小鼠减少。在小鼠和女性中的研究表明在中国内膜异位病损发展过程中,TGF-β配体水平升高与腹膜中免疫细胞活性下降有关,伴随异位子宫内膜细胞存活、黏附、侵袭和增殖均增加。TGF-β1与异位子宫内膜和腹膜细胞的代谢、
血管生成的起始以及子宫内膜异位病损的进一步进展均相关。表明TGF-β1在腹膜子宫内膜异位病损的进展中发挥重要作用,此外,针对这一信号通路或许是一种有效的治疗。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#子宫内膜异位#
33
#内膜#
22
很全面(^_^)
50
比较全面.学习了.谢谢!
41
#研究进展#
38
学习了受益匪浅
0