JCO:西妥昔单抗升级剂量治疗转移性结直肠癌
2012-07-30 卢秀玲 医学论坛网
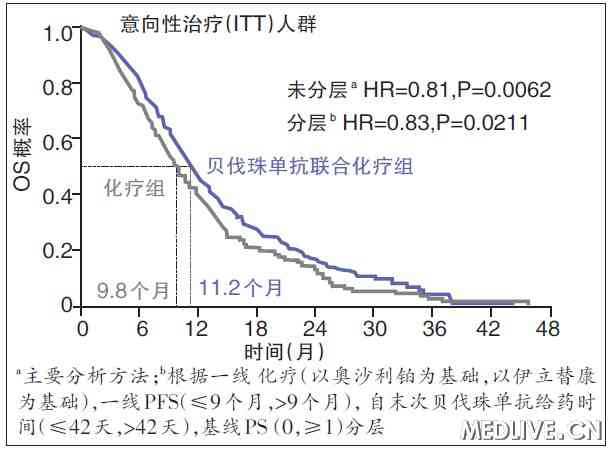
《临床肿瘤学杂志》(Journal of Clinical Oncology)于2012年7月2日在线发表的一项随机EVEREST研究表明,对于伊立替康-难治性转移性结直肠癌患者,采用西妥昔单抗升级剂量治疗或较标准剂量更有效。 人们认为,在若干肿瘤类别中,患者服用西妥昔单抗出现的皮肤毒性与临床转归呈正相关。本试验研究了对于伊立替康-难
链接;
Van Cutsem E,Tejpar S,Vanbeckevoort D,Peeters M,Humblet Y,Gelderblom H,Vermorken JB,Viret F,Glimelius B,Gallerani E,Hendlisz A,Cats A,Moehler M,Sagaert X,Vlassak S,Schlichting M,Ciardiello F.Intrapatient Cetuximab Dose Escalation in Metastatic Colorectal Cancer According to the Grade of Early Skin Reactions: The Randomized EVEREST Study.J Clin Oncol 2012 Jul 2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#西妥昔#
28
#JCO#
44
#转移性#
38
#结直肠#
34