J. Exp. Med.:阻断CDK蛋白可导致三阴性乳腺癌萎缩
2012-04-10 towersimper 生物谷
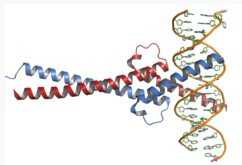
根据PDB文件1nkp而构建出c-Myc(红色)与Max(蓝色)和DNA形成的复合物的结构。图片来自维基共享资源。 根据2012年3月9日发表在Journal of Experimental Medicine期刊上的一篇研究论文,抑制一种大量存在的促进生长的蛋白能够导致三阴性乳腺癌消退。 三阴性乳腺癌(triple-negative breast tumor)缺乏其他类型乳腺癌中存在的所有已知

根据PDB文件1nkp而构建出c-Myc(红色)与Max(蓝色)和DNA形成的复合物的结构。图片来自维基共享资源。
根据2012年3月9日发表在Journal of Experimental Medicine期刊上的一篇研究论文,抑制一种大量存在的促进生长的蛋白能够导致三阴性乳腺癌消退。
三阴性乳腺癌(triple-negative breast tumor)缺乏其他类型乳腺癌中存在的所有已知的可以作为治疗靶标的生长受体,这样也就使得它成为乳腺癌中最难治疗的疾病亚型。患上这种癌症的病人往往有着更短的无疾病存活期,而且肿瘤在他们身上也容易更早地复发。
如今,Andrei Goga和同事们发现三阴性乳腺癌表达高水平的促进生长的MYC蛋白。MYC活性是这些侵袭性肿瘤生长所必需的,因而阻断一种MYC协作性蛋白(MYC-cooperating protein),即CDK,导致小鼠中三阴性乳腺癌萎缩。
归纳在一起,这些结果鉴定出一种新的潜在性靶标用于治疗三阴性乳腺癌。(生物谷:towersimper编译)

doi:10.1084/jem.20111512
PMC:
PMID:
MYC pathway activation in triple-negative breast cancer is synthetic lethal with CDK inhibition
Dai Horiuchi, Leonard Kusdra, Noelle E. Huskey, Sanjay Chandriani, Marc E. Lenburg, Ana Maria Gonzalez-Angulo, Katelyn J. Creasman, Alexey V. Bazarov, James W. Smyth, Sarah E. Davis, Paul Yaswen, Gordon B. Mills, Laura J. Esserman, and Andrei Goga
Estrogen, progesterone, and HER2 receptor-negative triple-negative breast cancers encompass the most clinically challenging subtype for which targeted therapeutics are lacking. We find that triple-negative tumors exhibit elevated MYC expression, as well as altered expression of MYC regulatory genes, resulting in increased activity of the MYC pathway. In primary breast tumors, MYC signaling did not predict response to neoadjuvant chemotherapy but was associated with poor prognosis. We exploit the increased MYC expression found in triple-negative breast cancers by using a synthetic-lethal approach dependent on cyclin-dependent kinase (CDK) inhibition. CDK inhibition effectively induced tumor regression in triple-negative tumor xenografts. The proapoptotic BCL-2 family member BIM is up-regulated after CDK inhibition and contributes to this synthetic-lethal mechanism. These results indicate that aggressive breast tumors with elevated MYC are uniquely sensitive to CDK inhibitors.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#阻断#
35
#萎缩#
22
#阴性乳腺癌#
21
#CDK#
37
#三阴性#
33
#Med#
29