Neuro-Oncology:纳米技术治疗致死性脑肿瘤
2012-04-10 Beyond 生物谷
在过去的40年中,辐射一直是治疗致命的脑瘤即胶质母细胞瘤最有效的方法。但是,虽然定位技术已得到改进,辐射光束仍然必须通过健康的脑组织才能到达肿瘤部位,患者在出现严重副作用之前只能容忍少量的辐射。 近日,圣安东尼奥得克萨斯大学健康科学中心大学的研究人员开发出一种能将纳米粒子辐射直接递送到脑肿瘤部位,并将其保持在肿瘤部位。该方法使得肿瘤本身接受到高水平的辐射,其辐射剂量是目前癌症患者放射治疗剂量
在过去的40年中,辐射一直是治疗致命的脑瘤即胶质母细胞瘤最有效的方法。但是,虽然定位技术已得到改进,辐射光束仍然必须通过健康的脑组织才能到达肿瘤部位,患者在出现严重副作用之前只能容忍少量的辐射。

近日,圣安东尼奥得克萨斯大学健康科学中心大学的研究人员开发出一种能将纳米粒子辐射直接递送到脑肿瘤部位,并将其保持在肿瘤部位。该方法使得肿瘤本身接受到高水平的辐射,其辐射剂量是目前癌症患者放射治疗剂量的20到30倍,同时该技术并不会影响脑部其它大面积的健康组织。
该研究最近发表在Neuro-Oncology杂志上,实验室研究获得成功结果已经足够让他们着手准备开始在癌症治疗和研究中心开展一项临床试验,该研究报告的通讯作者、CTRC神经肿瘤科专家Andrew Brenner医学博士将会主持这项临床试验。
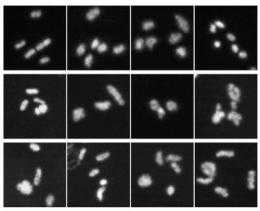
Brenner博士说:我们发现可以在动物模型中使用更高的辐射剂量,动物实验中这一剂量很安全,同时能够完全消除肿瘤。辐射由铼-186的同位素产生,铼-186半衰期很短。一旦放置在肿瘤内,铼发出的辐射能延伸出几毫米。
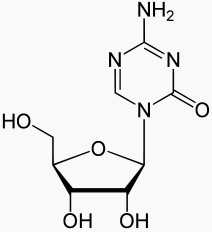
但是简单地把铼放入脑瘤中,由于微小颗粒(铼)将很快被血流清除,无法将铼保留在脑瘤组织内,因而铼将无法发挥正常工作。这个问题由解决核医学医师William T. Phillips医师和放射科的生物化学家Beth A. Goins博士、医疗物理学家和耳鼻咽喉科的Ande Bao博士以及所有德克萨斯大学健康科学中心医学部的医药化学家共同合作完成。他们将铼封装在微乎其微的脂肪分子或脂质体中(约100纳米宽)。
Brenner博士说:“这项技术是独一无二的,只有我们可以让这些脂质体拥有很高水平的放射性。
医生们希望夏季来临的时候就能开展临床试验。(生物谷:Bioon)

doi:10.1093/neuonc/nos060
PMC:
PMID:
Rhenium-186 liposomes as convection-enhanced nanoparticle brachytherapy for treatment of glioblastoma.
Yasmin M Ramdzan, Saskia Polling, Cheryl P Z Chia, Ivan H W Ng, Angelique R Ormsby, Nathan P Croft, Anthony W Purcell, Marie A Bogoyevitch, Dominic C H Ng, Paul A Gleeson, Danny M Hatters.
Although external beam radiation is an essential component to the current standard treatment of primary brain tumors, its application is limited by toxicity at doses more than80 Gy. Recent studies have suggested that brachytherapy with liposomally encapsulated radionuclides may be of benefit, and we have reported methods to markedly increase the specific activity of rhenium-186 (186Re)–liposomes. To better characterize the potential delivery, toxicity, and efficacy of the highly specific activity of 186Re-liposomes, we evaluated their intracranial application by convection-enhanced delivery in an orthotopic U87 glioma rat model. After establishing an optimal volume of 25 μL, we observed focal activity confined to the site of injection over a 96-hour period. Doses of up to 1850 Gy were administered without overt clinical or microscopic evidence of toxicity. Animals treated with 186Re-liposomes had a median survival of 126 days (95% confidence interval [CI], 78.4–173 days), compared with 49 days (95% CI, 44–53 days) for controls. Log-rank analysis between these 2 groups was highly significant (P = .0013) and was even higher when 100 Gy was used as a cutoff (P < .0001). Noninvasive luciferase imaging as a surrogate for tumor volume showed a statistically significant separation in bioluminescence by 11 days after 100 Gy or less treatment between the experimental group and the control animals (χ2[1, N= 19] = 4.8; P = .029). MRI also supported this difference in tumor size. Duplication of tumor volume differences and survival benefit was possible in a more invasive U251 orthotopic model, with clear separation in bioluminescence at 6 days after treatment (χ2[1, N= 9] = 4.7; P = .029); median survival in treated animals was not reached at 120 days because lack of mortality, and log-rank analysis of survival was highly significant (P = .0057). Analysis of tumors by histology revealed minimal areas of necrosis and gliosis. These results support the potential efficacy of the highly specific activity of brachytherapy by 186Re-liposomes convection-enhanced delivery in glioma.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Oncology#
37
#Oncol#
37
#脑肿瘤#
39
#纳米技术#
36
#致死性#
46