ESH2018丨SGLT-2抑制剂对于合并糖尿病的高血压患者之影响
2018-06-17 国际循环编辑部 国际循环
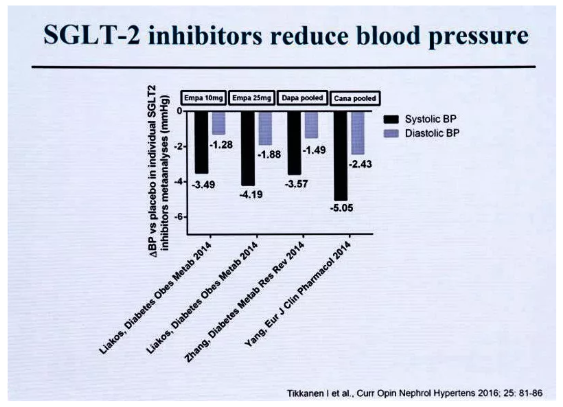
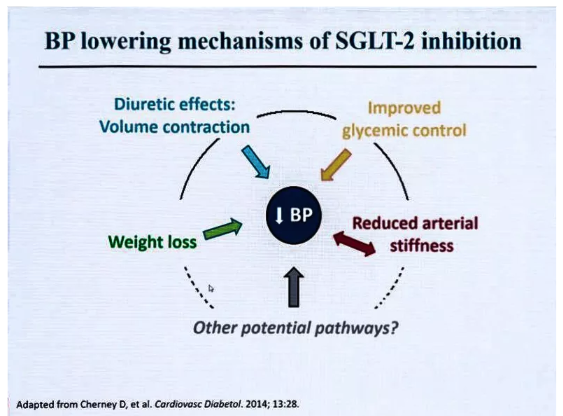
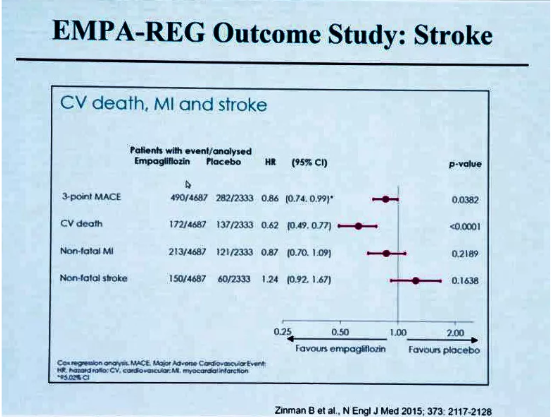
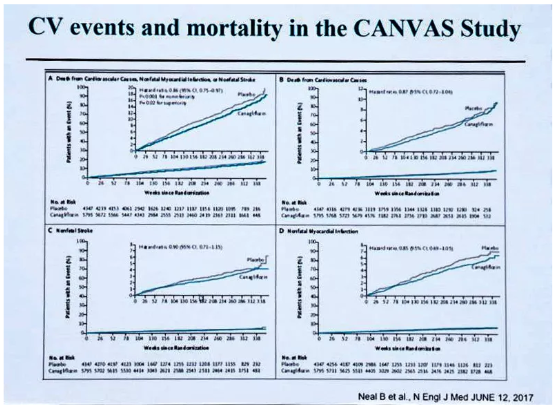
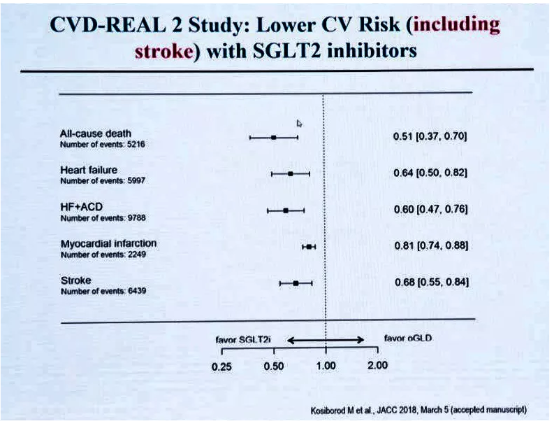
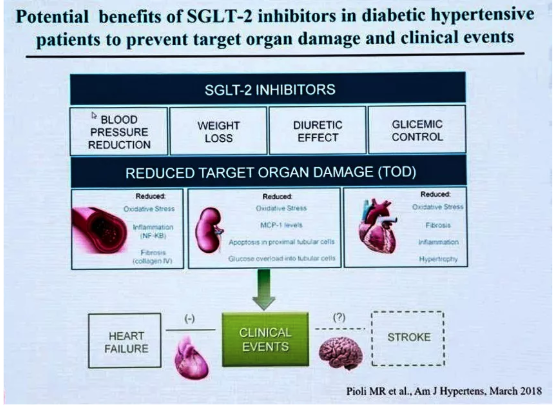
心血管及肾脏并发症是2型糖尿病患者的重要并发症,人们一直在积极寻求既能降糖又能降低心血管及肾脏并发症的药物。从近年来的相关研究结果来看,SGLT-2抑制剂似乎在这方面取得不错的结果。2018年6月9日西班牙当地时间下午,在ESH 2018年会“热点话题专题研讨会:2型糖尿病——需多学科干预来预防心血管并发症”专场上,来自芬兰赫尔辛基大学的IlkkaTikkanen教授作了专题讲座,解析了SGLT-

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#SGLT-2#
45
#SGLT#
33
#抑制剂#
36
#SGLT-2抑制#
42
#2抑制剂#
34
糖尿病患者高血压并发症扩大
47
该药应该是预防糖尿病患者合并症的一个里程碑药物.
69
#高血压患者#
26
#ESH#
34