Stroke:高hsCRP水平可预测卒中复发和不良功能预后
2016-06-29 phylis 译 MedSci原创
背景和目的:轻型脑卒中和短暂性脑缺血发作后,致残性卒中的发生率较高。研究者旨在探讨超敏C反应蛋白(hsCRP)预测卒中复发和不良功能预后中的作用。方法:在急性非致残性脑血管事件高危患者氯吡格雷试验中(CHANCE),来自73个(64%)预先设定的中心3044例(59%)患者,测定其hsCRP水平。主要预后为90天内发生卒中。次要预后包括联合血管事件和残疾或死亡(定义为90天改良Rankin量表评分
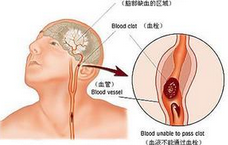
背景和目的:轻型脑卒中和短暂性脑缺血发作后,致残性卒中的发生率较高。研究者旨在探讨超敏C反应蛋白(hsCRP)预测卒中复发和不良功能预后中的作用。
方法:在急性非致残性脑血管事件高危患者氯吡格雷试验中(CHANCE),来自73个(64%)预先设定的中心3044例(59%)患者,测定其hsCRP水平。主要预后为90天内发生卒中。次要预后包括联合血管事件和残疾或死亡(定义为90天改良Rankin量表评分2到6)和1年随访中,新的血管事件发生。应用Cox比例风险模型和Logistic回归模型分析hsCRP与卒中复发和功能预后的相关性。
结果:研究人群中,32%的患者出现超敏C反应蛋白升高(>3mg/L)。随访90天内,与hsCRP<1 mg/L相比,hsCRP>3 mg/L的患者卒中复发(aHR,1.46;95%CI,1.08-1.98;P = 0.039),缺血性脑卒中及联合血管事件发生风险增加,不良功能预后差(aHR,1.68;95%CI,1.22-2.32;P = 0.002)。高hsCRP水平也可预测1年随访期间卒中复发。hsCRP水平与随机抗血小板治疗没有相互作用。
结论:在急性轻型卒中或短暂性脑缺血发作患者中,高hsCRP水平预测卒中复发和不良预后。
原始出处:
Li J, Zhao X, et al. High-Sensitive C-Reactive Protein Predicts Recurrent Stroke and Poor Functional Outcome: Subanalysis of the Clopidogrel in High-Risk Patients With Acute Nondisabling Cerebrovascular Events Trial. Stroke. 2016 Jun 21.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#HSC#
36
#CRP水平#
32
#CRP#
34
#卒中复发#
41
#功能预后#
33
#SCR#
0