关注|中国经自然腔道取标本术唱响音乐之乡
2018-05-30 王贵玉 医师报
美国结直肠外科医师协会(ASCRS)是北美地区结直肠外科医师的官方机构,肩负着结直肠专科医师培训、考核、继续教育等任务。5月19~23日,ASCRS在美国纳什维尔举行年会,作为北美地区结直肠外科领域的年度盛会,大会涵盖了结直肠外科的最新进展、专科医师培训、继续教育、患者健康管理等诸多方面的内容。
美国结直肠外科医师协会(ASCRS)是北美地区结直肠外科医师的官方机构,肩负着结直肠专科医师培训、考核、继续教育等任务。5月19~23日,ASCRS在美国纳什维尔举行年会,作为北美地区结直肠外科领域的年度盛会,大会涵盖了结直肠外科的最新进展、专科医师培训、继续教育、患者健康管理等诸多方面的内容。本次大会吸引全世界结直肠外科领域的专家学者积极参与。中国结直肠外科医生向与会者介绍了我国在经自然腔道取标本手术(NOSES)领域的新技术,得到参会专家和代表的认可,令人鼓舞。
哈尔滨医科大学附属第二医院结直肠肿瘤外科——王贵玉教授受邀出席本次盛会。并带来了中国学者的声音,王贵玉教授团队的手术视频“腹部无辅助切口经阴道拖出标本的右半结肠癌根治术”被评为优秀手术视频,在手术录像展播厅循环展播。本次也是王贵玉教授团队NOSES手术再一次在国外重要学术会议的展示,展现中国学者的微创理念和手术技巧。
NOSES属于微创中的微创,为微创治疗找到了的新方向。NOSES的定义是“使用腹腔镜器械、经肛门内镜(TEM)或软质内镜等设备完成腹腔内手术操作,经自然腔道(直肠、阴道或口腔)取标本的腹壁无辅助切口手术,术后腹壁仅存留几处戳卡疤痕。”可开展NOSES术的组织器官主要有结直肠、胃、小肠、肝胆及妇科肿瘤等。该技术通过使用常规微创手术器械,结合独特的消化道重建方式,以及标本取出途径,既保证了肿瘤的根治性切除,同时也能达到最佳的微创效果。
据悉,除了非常吸引人的录像展播环节外,ASCRS年会还采用主题发言并现场提问和评论、专家论坛、电子壁报展览、主题讨论辩论,主题培训等多种交流形式。有针对高年资医师的“workshop”手把手教学课程;以及青年医师培训课程,包括面试技巧等实用内容。
本次大会对于专业严谨执着的精神也同时体现在一些特殊的环节,包括缅怀在结直肠专业领域做出过突出贡献的大师级医生,并且在人文关怀和医学伦理等方面设置了专题研讨。
2018ASCRS | 美国结直肠外科医师年会会讯
四大亮点引爆ASCRS年会
▲哈尔滨医科大学附属第二医院结直肠肿瘤外科 王贵玉 发自美国纳什维尔
亮点一:直肠阴道瘘治疗建议
直肠阴道瘘治疗棘手,术后易复发,严重影响患者的生活质量。来自加利福尼亚州的Elizabeth Raskin教授强调,在直肠阴道瘘的初始评估和治疗中,必须首先了解病理学特点,如隐窝感染脓肿,炎症性肠病(IBD)或恶性肿瘤等。疾病活动期或感染状态时,治疗常失败。还应注重肛门括约肌功能评价,肛门功能将影响治疗方式的选择;英国的Phil Tozer教授介绍瘘的最新治疗方法,包括干细胞、生物材料、FiLaC?(瘘管激光闭合)、VAAFT(视频辅助瘘管治疗)等技术。
结合最新ASCRS指南和年会内容,笔者将相关治疗推荐做一总结:
产伤相关直肠阴道瘘、其他良性和症状轻微瘘均可保守治疗(2C)。产伤直肠阴道瘘可先保守治3~6个月。挂线引流有助于控制直肠阴道瘘相关的急性炎症或感染(1C)。
挂线引流可防止形成直肠阴道间隔脓肿,尤其是瘘管狭窄,阴道侧开口直径小,多个窦道者。对无法手术者,也有助于长期缓解症状。炎症、肿瘤或瘘的综合治疗前,挂线可控制急性炎症和感染,使后续治疗成功率更高。如挂线不能控制相关症状、炎症或感染时,可行转流性造口。
简单的直肠阴道瘘可选直肠推进瓣修补术(1C)。利用部分直肠壁皮瓣覆盖直肠阴道隔的缺损,最常用于修复简单的直肠阴道瘘,如合并肛门括约肌功能障碍,可行括约肌成形术。经会阴瘘管切开缝合术(EP)可治疗伴有严重肛门括约肌损伤的直肠阴道瘘患者(1C)。
将阴道瘘切开,转为类似Ⅳ度会阴裂伤,再依次缝合直肠黏膜、肛门括约肌、阴道黏膜及会阴皮肤,可治疗直肠阴道瘘伴严重肛门括约肌缺损排便失禁者,治愈率78%~100%,且肛门功能良好。其优点是同期修复括约肌,但手术复杂创伤大,需有经验的医生开展。对复发或复杂直肠阴道瘘,可用股薄肌或球海绵体肌(Martius术)转移修补术(1C),通常需转流性造口。
结肠直肠吻合并发症引起的高位直肠阴道瘘通常需经腹修补(1C)。低位直肠癌手术并发直肠阴道瘘的比例达10%。通常推荐转流性造口为初始治疗,控制感染,有些患者可治愈。
转流治疗失败,可重新行结肠直肠吻合、直肠推进瓣修补术,或臀部皮瓣修补术。放疗相关、复杂性、复发直肠阴道瘘,可能需要直肠切除,结肠下移或行结肠肛管吻合治疗(2C)。盆腔放疗导致的直肠阴道瘘,可以用转移肌瓣修补,袖状切除病变直肠肠管,结肠肛管吻合,或行预防性造口,同期或分期结肠肛管吻合。
以上列出一些治疗直肠阴道瘘的方法,仍缺乏高级别证据的支持。
亮点二:新颖的TaTME手术尚需完善
经肛门直肠全系膜切除术(TaTME)是近年学者们提出的一项新的手术方式。该种术式结合了直肠全系膜切除的原则和经肛门微创手术的理念,采用自下而上的手术方式,经肛门完成直肠全系膜切除。TaTME可以说是一项具有前景的技术。目前多数的研究都显示了TaTME的优势。本次会议主要分析了TaTME在美国应用的不足之处,并对TaTME的演变进行了介绍;开展了基于TaTME解剖内容的理论和实践操作的内容;TaTME视频展示和讲解。
与腹腔镜直肠全系膜切除术相比,美国学者认为TaTME具有更佳的手术视野,更完整的系膜切除,更好的短期疗效。但作为正在发展中的TaTME技术也存在一些缺点:
(1)关于TaTME疗效的评估,大多数为回顾性研究和病例对照研究,缺少多中心的随机对照试验;(2)国内外开展TaTME手术的均为大规模、高级别的医学中心,在规模较小的地区医院尚未开展。
(3)TaTME手术操作步骤多种多样,并不统一。这就给疗效的评估带来了很大的挑战。
(4)TaTME手术必须要经肛门操作,这就离不开新的手术设备,也就是经肛门操作平台。目前外科医生有的利用TEM平台辅助,有的利用腹腔镜设备辅助,会带来不同的手术视野和操作空间,因此要有统一的经肛门操作平台,才能更好的评价手术疗效。
(5)TaTME手术尚无明确的适应证。目前正在进行的随机对照临床试验COLOR Ⅲ研究提出的适应证:T3期肿瘤,环周切缘小于1 mm,且肿瘤未侵袭肛门内括约肌和肛提肌。在此研究中,TaTME手术的适用人群非常有限。TaTME手术能否适用范围更大的人群,还需探讨;(6)在手术相关的短期临床疗效中,TaTME已经存在优于传统腹腔镜手术的趋势。但是目前的研究,还缺少对长期疗效的评价。这些长期的因素包括,肿瘤患者的长期生存情况以及患者的肛门功能。
尽管TaTME有一定的优势,但尚不完善,对于一项新颖的手术技术,我们要秉持严谨审慎的态度。在肯定进步的同时,要认识到不足,从而合理化评价TaTME手术,为患者带来更多的获益。

2018ASCRS会议现场
亮点三:疫苗接种让肛门上皮内瘤变者受益
肛门上皮内瘤变(AIN)是肛门黏膜的一种癌前病变,是肛门癌的前兆。在美国尽管肛门癌十分罕见,但这种恶性肿瘤的发生率也在持续上升,在某些高危人群中,肛门癌的发生率可能会超过大肠癌。AIN和大肠癌的高危因素包括临床因素、人类乳头瘤病毒(HPV)感染和持续感染的相关途径的行为。而HPV感染最强的相关危险因素是人类免疫缺陷病毒(HIV)感染、肛交和高危性行为。由HPV介导的生殖器官癌症的研究历史表明,感染HPV病毒株是导致AIN/肛门癌的另一种高危因素。因此在本次ASCRS年会上,针对HPV和AIN的关系也成为了一大讨论热点。会议主要从HPV研究中的问题、病理学和细胞学研究、AIN诊断等方面进行了研讨。
高危人群应常规筛查
AIN进展为肛门癌发生在一些个体身上已经有多年。对AIN和肛门癌的筛查以及对晚期AIN病变的治疗,在某些高危人群中是很合理的。尽管缺乏筛查和治疗结果的随机对照试验,但专家仍支持对高危人群进行常规筛查。通过肛门细胞学的检查进行筛查,类似于在宫颈癌筛查项目中进行的检查,以及通过高分辨率肛门镜(HRA)进行评估和直接组织学活检。AIN可以通过使用咪喹莫特、5-氟尿嘧啶和三氯乙酸等进行局部治疗,也可以选择电灼烧、激光等消融治疗。有研究表明,在高危人群接种疫苗来预防HPV病毒的研究中,AIN和肛门癌的发生率下降。
专家建议在高危人群中应考虑对AIN和早期肛门癌的筛查,以及对这些相关病变的治疗。通过肛门细胞学活检及HRA进行筛查,治疗包括局部治疗和消融治疗。而HPV疫苗的接种在一定程度上似乎降低了AIN和肛门癌的发病率。
AIN是肛门鳞状细胞癌的癌前病变。尽管认为AIN在一部分患者中进展为SCC,但进展的风险仍不清楚。
有证据表明,某些高危人群的进展风险升高,包括:(1)持续感染高危型HPV病毒株的患者;(2)HIV阳性的患者,特别是CD4计数低者;(3)与男性发生性关系的男性(MSM);(4)HPV感染引起的生殖器官癌症(特别是宫颈癌)。这些群体将可能受益于加入正式的AIN筛查项目。
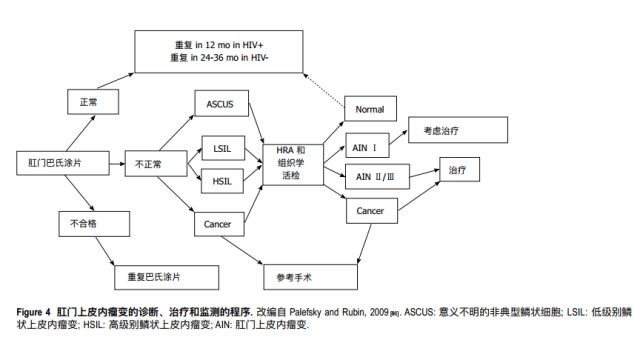
肛门上皮内瘤变的诊断、治疗和监测的程序
专家共识至关重要
AIN对诊断和治疗可能具有挑战性,因此可转诊至能够解释细胞学和病理学、进行HRA和治疗AIN的专家中心是至关重要的。最佳的治疗方式和时间间隔目前尚未确定,而且建议主要基于专家共识,并由当地专家推动。无论治疗方式如何,高级别AIN的复发率都很高,建议对有AIN病史的患者进行持续的监测。新的成像技术可以不需要组织学活检就能识别高危病变。
共聚焦激光显微镜(CLSM)已被证明至少与组织学活检一样有效,用于检测食管表面的鳞状细胞癌,可能对AIN的检测和分级同样有效。还需要进一步研究来确定CLSM在AIN中治疗的作用和功效。
综上所述,AIN是一种临床上重要的病变,许多临床医生经常不予以重视。虽然肛门癌仍然相对少见,但这种恶性肿瘤的发病率正在增加。随着有效的HPV疫苗普及,临床医生必须了解AIN,特别是在高危人群中,他们可能在接种疫苗中获益最多。
亮点四:成人先天性巨结肠 腹腔镜辅助手术显优势
成人先天性巨结肠症(AHD)系小儿先天性巨结肠症(HD)的迁延和缓发,是一种少见疾病。约占先天性巨结肠症的 4%~5%。多数患者在幼儿时期即有慢性便秘或腹胀,但症状较轻,未予诊治,随年龄的增长,症状渐重。成年后多因肠梗阻入院治疗。Alessandra Gasior 教授对这一疾病进行了详细阐述。AHD 必须明确诊断,否则手术处理会出现问题。
六大问题值得注意
如能追问到胎粪排出延迟病史,对诊断有参考价值;长期便秘是 AHD 的主诉,可追诉到幼年时;因此,在便秘病因不能解释时应考虑AHD。
长期便秘突然发生结肠梗阻并腹部触及粪石着,不应只行肠切开取粪石,而应寻找引起梗阻的病因。
在外院诊断 HD 并行根治手术者,如术后仍严重便秘,应详细询问及查阅手术记录,可能没有达到 HD 根治性手术;如无神经节细胞的直肠留得过长,甚至根本没有切除,拖出的近端结肠可能是移行段甚至痉挛段,也可能是吻合口狭窄。
钡剂灌肠结肠造影是诊断 ADH 的常用方法,摄片应包括全部骶椎和肛门标记。 ADH 短段型多见,如果骶椎和肛门标记未显示,则无法对 HD 进行分型甚至漏诊。
肛门直肠测压是诊断 AHD 的重要方法,其特征性改变是直肠肛门抑制反射消失,同时可评价术后便秘的其他原因。
诊断困难的患者可做直肠黏膜肌层活检和乙酰胆碱酯酶测定。
外科术式需个体化
AHD 的治疗分为保守内科治疗和外科手术治疗,但是 AHD 患者往往是因内科保守治疗无效就诊。AHD 手术治疗的术式主要有:
Swenson 术式:经腹游离直肠至齿状线上 2 cm ,切除无神经节细胞的肠管后端端吻合;此手术可能会引起尿失禁、大便失禁和性功能障碍。
Duhamel 术式:仅切除腹腔内病变肠段,完整保留直肠,在直肠和骶骨间分离出一腔隙,拖出肠管与直肠侧侧吻合,但是由于保留了部分无神经节细胞的直肠,术后出现特有的闸门综合征和反复发作的小肠结肠炎。
Soave 术式:是做直肠黏膜层面的分离,保留直肠袖状肌层,减少对直肠周围组织的影响,但是由于 Soave 术式保留无神经节细胞的直肠肌鞘,术后会出现残留肌鞘导致的功能性梗阻和排空障碍。
腹腔镜辅助 Swens- on-like 手术:前壁保留 1.5~2 cm,后壁保 留 1 cm,其优势是:(1)可以充分游离结肠,确保无张力吻合;(2)能够完整保留拖下肠管的边缘 血管弓,保证吻合口血运良好;(3)尽量紧贴肠管的游离,最大限度减少对周围组织的影响,而且能够游离到接近齿状线上 1 cm水平,翻出并切开结肠,仍然是紧贴肠壁游离,不仅能够减少对周围组织的影响,而且保证肠壁切缘精准和完整;(4)全层对全层吻合,保证良好的对合;(5)吻合口呈斜行椭圆,吻合口狭窄发生率降低;(6)吻合口暴露良好,直视下精准缝合;(7)避免 Soave 手术肌鞘和 Duhamel 闸门相关 并发症。
总之,成人 HD 根治手术的术式选择首要的是患者结肠的病理状况,术式选择需个体化,手术者个人的临床经验也很重要。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#标本#
24
#音乐#
0
好文.值得点赞!认真学习了.把经验应用于实践.为患者解除病痛.
41
学习谢谢分享
0
好
44
学习学习再学习
44
学习了很有用不错
47