病例分析:婴幼儿Galen大脑大静脉瘤栓塞术 如何护理?
2017-04-18 王春雪,张宁 中国卒中杂志病例精选
1 病例简介患儿女,7岁,因“左侧肢体无力伴头痛、头晕3日,突然加重1日”于2009年3月27日坐轮椅入院。
1 病例简介
患儿女,7岁,因“左侧肢体无力伴头痛、头晕3日,突然加重1日”于2009年3月27日坐轮椅入院。患儿于2009年3月23日前开始出现左侧肢体无力,行走不稳,伴间断头痛、头晕,在当地医院颅脑CT平扫和增强提示大脑大静脉瘤伴轻度脑积水。2009年3月25日头痛持续性加重,并发呕吐,左侧肢体无力进展至完全不能动,转至我院治疗。
入院查体:体温36.7℃,脉搏98次/分,左侧肢体血压88/56mmHg,右侧肢体血压95/ 60mmHg,呼吸23次/分。神志清楚,精神差,体格发育正常,双肺听诊无干湿性啰音,心律齐,未闻及杂音,双侧桡动脉搏动对称,颈部血管未闻及杂音。神经系统查体:双侧瞳孔等大等圆,直径约2.0mm,对光反射灵敏,语言流利,颅神经查体无异常,左侧上肢肌力0级,左下肢1级,肌张力稍低,右侧上下肢肌力肌张力正常,感觉查体未见异常,颈软,无抵抗,双侧病理征(±)。
实验室检查:血常规、生化、凝血结果正常。
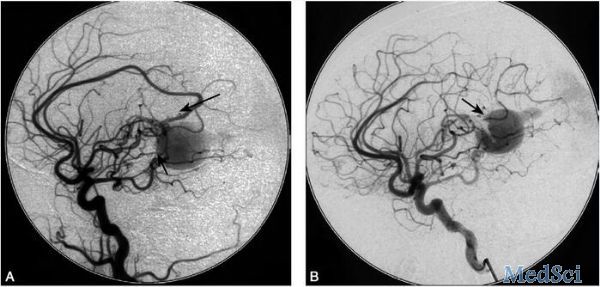
全脑血管DSA检查:大脑大静脉呈瘤样扩张,由左侧大脑前动脉、椎动脉及后交通动脉向其供血(图2.4-1)。
图2.4-1 Galen大脑大静脉瘤患儿全脑血管DSA检查结果
A.左颈总动脉正位术前(短箭头示大脑大静脉瘤样扩张,长箭头示左侧大脑前动脉向静脉瘤供血);B.左颈总动脉侧位术后(箭头示左侧大脑前动脉向静脉瘤的供血关闭)
诊疗经过:于2009年3月30日,在全麻下经动脉途径行静脉瘤栓塞术,选用α-氰基丙烯酸正丁酯(N-butyl 2-cyanoacrylate,NBCA)和弹簧圈栓塞左大脑前动脉、右椎动脉及后交通动脉瘘口处。最后造影显示脑供血良好,脑的静脉血液经正常的上矢状窦和直窦引流(图2.4-1)。术后持续监护,常规应用肝素,硝普钠持续降压和人工冬眠镇静,收缩压控制在90mmHg左右,严格控制液体入量等措施。两周后出院,出院时左侧上肢肌力恢复为2级,左下肢为3级,出院后持续随访,患儿病情逐渐好转,未再复发。
诊断:大脑大静脉瘤
2 讨论
Galen 大脑大静脉瘤临床上很少见,多发生在新生儿及婴幼儿期,约占颅内血管畸形1%[1],是一种危及儿童的较为少见的血管性疾病。除Galen大脑大静脉瘤外,还被称作大脑大静脉扩张、大脑大静脉瘘。它是由于动静脉短路,使高流量的动脉血通过动静脉之间的瘘道直接冲击大脑大静脉;或后天的因素硬膜静脉窦狭窄、闭塞、缺如,造成流出道梗阻,使其瘤样扩张。扩张的静脉压迫大脑导水管,同时由于颅内静脉高压,引起脑脊液循环和吸收障碍而产生脑积水、颅内压增高的一系列症状,致残率和死亡率很高。临床表现可因年龄不同而异。婴儿期由于导水管受压而出现以脑积水为主的临床症状,可以伴有癫痫发作,有时颅内可听到血管性杂音[2]。由于“盗血”产生肺动脉高压和慢性脑缺血,可引起心功能不全和智力低下,很多并发心功能不全的患儿因未得到及时的诊治在婴幼儿期死亡。该病内科治疗无效,外科治疗难度大、风险高,目前公认血管内栓塞治疗效果最好,并且比较安全[3,4]。大脑大静脉瘤临床病例少,但病情重且并发症多,且婴幼儿患儿多,临床护理观察非常重要,所以对护理的要求高。
2.1 术前护理
2.1.1 心理护理
患儿年龄小,给予安置于单人间,父母陪护。严格限制探视,保持病房安静。通过图书、讲故事等交流形式,与患儿建立良好的护患关系,消除其紧张、恐惧心理,稳定情绪,以取得与医护的配合。对患儿父母进行健康教育,告知绝对卧床休息的重要性,避免激惹哭闹引起血压升高造成瘤体破裂出血。
2.1.2 严密监测病情
注意有无瘤体破裂出血症状、癫痫发作的先兆及四肢活动障碍情况。完善术前检查,术前8小时禁食水。记录患儿血压、视力、肢体活动及足背动脉搏动情况,以便术后对照。
2.1.3 术前用药
按医嘱术前24小时持续静脉注射尼莫地平,持续监测血压,根据血压调节滴速,收缩压控制在90mmHg左右,防止因输入过快,造成血压过低,而致脑血流灌注不足。术前30分钟按医嘱给予苯巴比妥钠50mg肌注。
2.2 术中护理
由护理人员陪送患儿到导管室。术中护理包括:①留置尿管,监测患儿的瞳孔、血压、脉搏及肢体活动情况,及时向手术医师汇报;②注胶栓塞后立即检查患儿,如发现血压不稳、呼吸异常、抽搐等症状及时汇报并按医嘱采取相应的处理措施。
2.3 术后护理
2.3.1 术后护理常规
观察患儿意识、生命体征及穿刺部位有无出血、渗血情况。穿刺部位予1kg沙袋加压包扎6小时,穿刺侧肢体制动8小时,卧床24小时,勿剧烈晃动头部,保持情绪稳定及大小便通畅,必要时使用约束带。监测血压,观察双下肢的足背动脉搏动、皮肤温度、颜色、血液循环(趾体色泽、趾温)、痛触觉情况,与术前比较,如有异常及时报告医师处理。
术后4~6小时如无呕吐可给予多饮水以促进造影剂排出。多吃蔬菜和水果,避免食用甜食、鸡蛋、豆浆等,防止便秘和胀气。多与患儿及家属交流,询问患儿有无不适感。患儿需严格平卧24小时,穿刺肢体处制动,可能引起背痛难忍,给予向患侧翻身60°,健侧翻身20°~30°,交替更换体位,保持患侧髋关节伸直,对侧下肢自由弯曲。尿管于术后2日拔除,拔管前夹闭尿管做膀胱充盈功能训练,拔管后观察患儿排尿情况。
2.3.2 术后血压控制及人工冬眠
术后24~72小时控制收缩压在90mmHg左右。为了保持血压的稳定以及预防癫痫的发生,术后24小时对患儿进行人工冬眠:生理盐水46ml加盐酸氯丙嗪50mg和盐酸异丙嗪50mg,以3~4ml/h持续泵入,使患儿保持在呼之能醒的安静状态。术后连续3日给予苯巴比妥钠50mg肌肉注射,每8小时1次,预防癫痫。注意观察癫痫发作先兆,一旦发作及时控制。使患儿成功度过术后危险期,本组病例冬眠效果理想,血压控制较好,无癫痫发生,情绪稳定。
2.3.3 头痛的护理
脑血管栓塞后,各种管道刺激血管引起脑血管痉挛以及脑积水致颅内压增高等,患儿于术后易出现头痛症状。术后用20%甘露醇快速静脉输注,连续3~6日。按每日液体总量30ml/kg,控制每日液体总量。积极治疗脑积水,降低颅压。同时静脉滴注尼莫地平,根据血压严格控制输入速度。严密观察患儿意识、瞳孔及生命体征的变化,注意头痛发生的时间、性质以及伴随的症状。发现异常及时通知医生进行处理。
2.3.4 肢体功能锻炼
患儿起病急,病情重,年龄小,且出现肢体功能障碍,患儿易出现恐惧心理,家属更担心预后。这时护士首先要建立良好的护患关系,及时进行心理疏导,为其制订早期康复计划,取得其配合。①良姿位的摆放:保证正确的卧床姿势,且经常更换体位,仰卧位由于受紧张性颈反射和迷路反射的影响,异常反射活跃,可以加重挛缩模式[5]。实际工作中,主要采取健侧卧位与平卧位交替,尽量减少患侧卧位,预防患肢受压受损。②被动运动和主动运动:有规律的运动瘫痪的关节,3~4次/日,每次每个动作10次左右,活动顺序由上至下,由大关节到小关节,循序渐进,幅度由小到大牵伸挛缩的肌肉、肌腱及关节周围组织,多做与挛缩方向相反的运动,直到主动运动恢复。③按摩:对肌张力高的肌群采取安抚性质的推摩使其放松,对肌张力低的肌群则予以擦摩和揉捏。
2.4 出院指导
经介入栓塞治疗,患儿病变血管破裂出血的风险减小,但并不等于疾病治疗的终止。告知患儿家属出院后继续行康复治疗;并让患儿注意休息,避免精神刺激和情绪激动;保持良好的生活习惯,饮食应低盐、易消化,注意少量多餐,保持大便通畅,避免用力排便,保证营养的摄入和良好的睡眠;避免单独外出,同时告知患儿定期门诊随访。
大脑大动脉瘤病例较少见,故临床护理经验少,而此类患者医疗措施复杂,也增加了护理的难度。我们通过对本病例的护理总结,以期为护理工作者在护理类似患者时提供一定的借鉴。
专家点评 刘佰运
Galen大脑大静脉瘤临床上很少见,多发生在新生儿及婴幼儿期。该病内科治疗无效,外科治疗难度大、风险高,目前公认血管内栓塞治疗效果最好。本文作者对病例进行了术前评估,制订了详细护理计划,并早期介入康复治疗,取得了令人满意的临床效果。由此可以看出,临床护理是一项既要求有扎实理论基础、丰富的临床经验,又需要科研创新能力的一项工作。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#静脉瘤#
43
#静脉#
38
学习了,很好的病例。
63
学习了,值得分享
55
学习了谢谢分享
0
难度大
65
学习了,多谢分享
63