JAMA Oncology:他汀类药物有助于接受雄激素剥夺疗法的前列腺癌患者延缓疾病进展
2015-05-08 Zhang JL译 MedSci原创
一项由丹纳-法伯癌症研究中心研究人员开展的临床试验结果显示,对不接受他汀类药物治疗的男性患者,在进行雄激素剥夺治疗后的前列腺癌患者接受降胆固醇的他汀类药物治疗能够获得更长时间的疾病控制。在这项最新在线发表在JAMA Oncology杂志上的研究中,研究人员报告说,在接受雄激素剥夺疗法(ADT)开始服用他汀类药物的男性患者平均27.5个月后疾病开始恶化,而没有接受他汀类药物治疗的男性则仅有17.4个
一项由丹纳-法伯癌症研究中心研究人员开展的临床试验结果显示,对不接受他汀类药物治疗的男性患者,在进行雄激素剥夺治疗后的前列腺癌患者接受降胆固醇的他汀类药物治疗能够获得更长时间的疾病控制。
在这项最新在线发表在JAMA Oncology杂志上的研究中,研究人员报告说,在接受雄激素剥夺疗法(ADT)开始服用他汀类药物的男性患者平均27.5个月后疾病开始恶化,而没有接受他汀类药物治疗的男性则仅有17.4个月。在参与这项试验的926名患者中,70%的患者在6年期间发生疾病进展。
“在延缓疾病进展方面的这平均10个月的获益表明,他汀类药物可能是我们目前的治疗前列腺癌宝贵的辅助药物,”该研究的第一作者、Dana-Farber生殖泌尿系肿瘤中心医学肿瘤学家Lauren Harshman博士说,“多项流行病学研究支持这一结果,表明他汀类药物的使用可能与前列腺癌预后的改善有关,但需要进一步验证。”
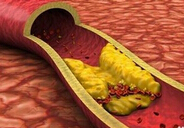
实验室试验的研究结果表明,他汀类药物可以延缓接受ADT治疗的前列腺癌患者的肿瘤生长速度。(ADT能够减少体内雄激素的量,防止前列腺癌细胞使用它来推动其进展。多年以来,它一直是激素敏感型前列腺癌扩散至前列腺体内阶段的一线治疗方式)。
在实验室研究阶段,研究人员把研究目标集中在一种叫做SLCO2B1的蛋白质,后者有助于各种药物和激素进入细胞。这些进入到细胞中分子的其中之一是硫酸脱氢表雄酮(DHEAS),后者是睾酮的前体,能够刺激前列腺癌细胞生长。类似地,他汀类药物也依靠SLCO2B1进入细胞。
在一系列的实验中,研究人员发现,他汀类药物可以在实验室培养的前列腺癌细胞系中干扰脱氢表雄酮的吸收。通过垄断SLCO2B1在前列腺肿瘤中的可用容量池(结合位点),他汀类药物基本上阻断了DHEAS进入癌细胞。临床研究结果表明这种方法可以对前列腺癌病人的治疗有效。
“我们的研究结果提出一个合理的机制,他汀类药物可能在前列腺癌细胞中通过减少肿瘤的雄激素池来改善患者的预后,”该研究的资深作者、Dana-Farber 生殖泌尿系肿瘤中心主任Philip Kantoff博士说,“需要进一步研究来验证我们的发现。”
原始出处:
1.Philip W. Kantoff, MD et al. Statin Use at the Time of Initiation of Androgen Deprivation Therapy and Time to Progression in Patients With Hormone-Sensitive Prostate Cancer. JAMA Oncology, May 2015 DOI: 10.1001/jamaoncol.2015.0829
2.Jorge D. Ramos, DO; Evan Y. Yu, MD. Progress in Understanding What Is Being Statin(ed) in Prostate Cancer. JAMA Oncology, May 2015 DOI: 10.1001/jamaoncol.2015.0833
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Oncol#
28
#Oncology#
28
#雄激素剥夺#
41
#疾病进展#
25
期待有更多研究
167
#他汀类药#
19
不错,不错
131