European Radiology:预测生存期的最佳反应时间点与肝细胞癌TACE术后的肿瘤负荷有关
2022-08-16 shaosai MedSci原创
初次TACE后的OR值更可能适用于小的单发结节,而大结节或多发结节通常需要重复TACE,最佳ORR变得更加直观准确。因此,肿瘤负荷这一特别的异质性特征会影响ORR评估预测生存的最佳时机。
 现阶段,经动脉化疗栓塞术(TACE)是不可切除的肝细胞癌(HCC)的推荐一线疗法,总生存期(OS)是评估预后的标准指标。然而,将OS作为唯一的终点会增加临床研究的难度。因此,根据修改后的实体瘤反应评价标准(mRECIST),客观反应(OR)被认为是另一种可靠的替代终点。
现阶段,经动脉化疗栓塞术(TACE)是不可切除的肝细胞癌(HCC)的推荐一线疗法,总生存期(OS)是评估预后的标准指标。然而,将OS作为唯一的终点会增加临床研究的难度。因此,根据修改后的实体瘤反应评价标准(mRECIST),客观反应(OR)被认为是另一种可靠的替代终点。
然而,重复 "按需 "进行TACE的普遍做法引起了一个问题,即OR的替代性是否应取决于初始手术后的反应(初始OR)或重复手术中取得的最佳反应(最佳OR)。目前,初始反应和最佳反应有时被括在一起预测生存率。然而,不同研究中评估反应的时间不一致,导致OR率(ORR)的变化影响了其代偿性。
初次TACE后的OR值更可能适用于小的单发结节,而大结节或多发结节通常需要重复TACE,最佳ORR变得更加直观准确。因此,肿瘤负荷这一特别的异质性特征会影响ORR评估预测生存的最佳时机。
近日,发表在European Radiology杂志的一项研究利用个体数据探讨了初始和最佳ORR的预后价值及其与肿瘤负荷的代偿性,为临床更准确的评估患者的治疗效果和评先分层提供了参考依据。
本研究于2010年1月至2016年5月期间对来自17家学术医院的共计1549名符合条件的不可切除的肝细胞癌(HCC)、Child-Pugh评分≤7、性能状态评分≤1的接受TACE治疗的患者进行了回顾性分析。根据 "6-12 "标准,如果最大肿瘤直径和肿瘤数量之和≤6,>6但≤12,以及>12,则肿瘤负担被分级为低、中和高。
初始和最佳ORRs均与肿瘤负荷相互影响。在低级别(调整后的HR分别为2.55和2.95,均为P<0.001;R=0.84,P=0.035,R=0.97,P=0.002)和中级别(调整后的HR分别为1.81和2.22,均为P<0.001;R=0.74,P=0.023,R=0.9,P=0.002)中,初始和最佳ORR可以等效地预测并与OS相关联。对于高级别,只有最佳ORR表现出合格的代偿性(调整后的HR,2.61,p<0.001;R=0.70,p=0.035),而初始ORR并不明显(调整后的HR,1.08,p=0.357;R=0.22,p=0.54)。
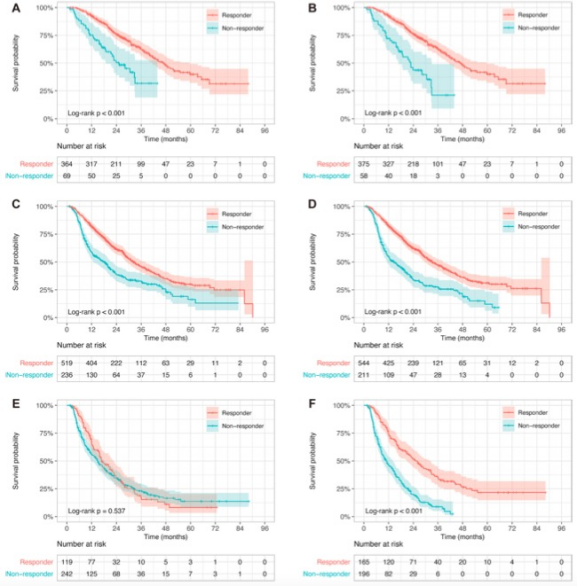
图 按肿瘤负荷分层的初始和最佳反应确定的反应者和非反应者的生存曲线。A 低肿瘤负荷层内初始应答者与非应答者的存活率。中位OS为47.2(41.2-59.6)个月,而非25.4(18.9-NA)个月,log-rank p < 0.001。B 低肿瘤负荷层中最佳反应者与无反应者的生存率。中位OS为47.2(41.6-59.6)个月与22.7(16.8-33.0)个月,log-rank p<0.001。C 初始应答者与中间肿瘤负荷层的非应答者的存活率。中位OS为32.1 (29.0-37.9) vs. 18.3 (12.7-22.2) 月,log-rank p<0.001。D 最佳反应者与无反应者在中等肿瘤负荷层中的生存率。中位OS为33.4 (29.5-38.5) vs. 14.6 (11.3-19.6) 个月,log-rank p < 0.001。E 高肿瘤负荷层内初始应答者与非应答者的存活率。中位OS为16.8(15.4-22.5)个月与14.9(12.0-18.2)个月,log-rank p = 0.537。F 高肿瘤负荷层内最佳反应者与无反应者的存活率。中位OS为24.8(20.9-32.5)个月与11.1(8.7-14.1)个月,log-rank p<0.001
本研究表明,评估ORR的最佳时机应根据肿瘤负担而定。对于Ts+Tn≤12的患者,在与最佳ORR相似的敏感性下,初始ORR的评估时机是最佳的。对于其余高肿瘤负荷的患者,虽然其预测价值不理想,但应首选最佳ORR,但仍不能忽视初始ORR在改变替代治疗策略中的价值。
原文出处:
Dongdong Xia,Qiuhe Wang,Wei Bai.Optimal time point of response assessment for predicting survival is associated with tumor burden in hepatocellular carcinoma receiving repeated transarterial chemoembolization.DOI:10.1007/s00330-022-08716-4
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
79
#TAC#
59
#细胞癌#
52
#ACE#
49
#肿瘤负荷#
43
#生存期#
51
#肝细胞#
46