糖尿病患者出现水肿,内分泌医生应该“肿么办”?
2017-03-26 于一江 医学界内分泌频道
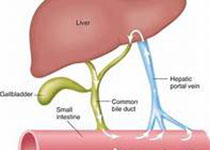
一糖尿病患者出现水肿,可能是因为以下病变水肿为组织间隙过量积液的一种病理现象,临床尤以下肢水肿最为常见。糖尿病人出现下肢水肿,除了少数原因外,大多与糖尿病的各种慢性并发症有关,常见以下情况:1、糖尿病并发心脏病糖尿病心脏病患者可因心功能不全(尤其是右心功能不全)引起体循环淤血及水钠潴留,导致颈静脉曲张、肝脾肿大及双下肢对称性水肿。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#分泌#
39
#水肿#
31
#糖尿病患者#
36
糖尿病并发症较多,应多加注意
53
写的内容很全面,实用
54
好好学习,涨知识
53
谢谢分享,学习了
49
临床很实用的资料
42
学习新知识谢谢分享
31
学习了很有用
25