Obstet Gyneco:多学科讨论 2009年指南更新后宫颈癌筛查过度与不足加剧
2017-04-18 韩茹,贾朝娟 环球医学资讯
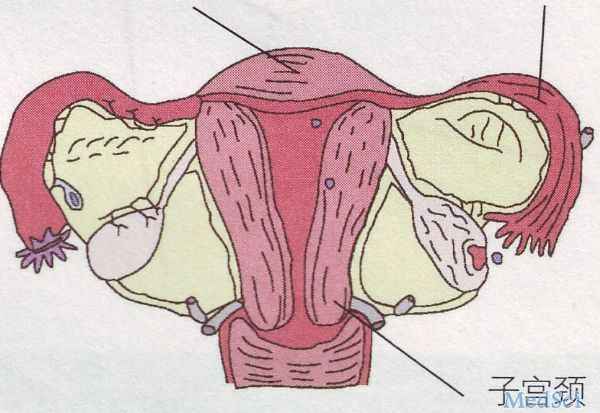
因宫颈癌的普遍筛查和治疗死亡率显著降低,但研究表明过度筛查包括操作带来的并发症、假阳性结果的治疗等也造成了伤害。2017年1月,发表在《Obstet Gynecol》的一项研究调查了宾西法尼亚Medicaid中2009年美国妇产科医生协会指南公布前后宫颈癌筛查的变化。研究结果显示,指南变更后宫颈癌过度筛查和过低筛查率均较高。请看本期多学科讨论组临床药师各抒己见为您梳理本文看点——目的:评估2009
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#TET#
19
#指南更新#
33
#NEC#
23
很好
57
#宫颈#
20
#多学科#
24
#宫颈癌筛查#
32
因宫颈癌的普遍筛查和治疗死亡率显著降低,但研究表明过度筛查包括操作带来的并发症、假阳性结果的治疗等也造成了伤害。
54
学习了谢谢分享
52
厉害了!
48