NEJM:Pembrolizumab用于晚期NSCLC展现出良好抗肿瘤活性(KEYNOTE-001研究)
2015-04-23 MedSci MedSci原创
来自Westwood Bowyer 癌症中心r的Edward B. Garon等在线发表在4月19日的《新英格兰医学杂志》上的研究显示:Pembrolizumab治疗晚期非小细胞肺癌患者具有抗肿瘤活性,且治疗时所发生的副反应在可接受的范围内。至少50%的肿瘤细胞出现PD-L1表达与pembrolizumab疗效提高具有相关性。 在一项一期研究中,研究者们对pembrolizumab抑制晚期非小细
来自Westwood Bowyer 癌症中心r的Edward B. Garon等在线发表在4月19日的《新英格兰医学杂志》上的研究显示:Pembrolizumab治疗晚期非小细胞肺癌患者具有抗肿瘤活性,且治疗时所发生的副反应在可接受的范围内。至少50%的肿瘤细胞出现PD-L1表达与pembrolizumab疗效提高具有相关性。
在一项一期研究中,研究者们对pembrolizumab抑制晚期非小细胞肺癌患者程序性细胞死亡-1(PD-1)的有效性和安全性进行了评估;我们还试图对与潜在临床疗效相关的PD-1配体1(PD-L1)的表达水平进行定义和验证。
研究者们将接受Pembrolizumab治疗的495例患者(剂量为每三周一次,每千克体重2mg或10mg;或每两周一次,每千克体重10mg)被分为两组:训练组(182例患者)和验证组(313例患者)。使用免疫组化分析法对肿瘤样本中PD-L1的表达情况进行评估,结果表述为膜性PD-L1染色肿瘤细胞的百分比(所占比例)。使用中间综述法每九周一次的对反应情况进行评估,如下。
pembrolizumab所致的常见副反应包括疲惫、瘙痒和食欲下降,且不会因用药剂量和方案不同而具有明显差异。所有的患者的客观反应率是19.4%,反应的中位持续时间为12.5个月,无疾病进展生存的中位持续时间为3.7个月,总生存期的中位持续时间为12.0个月。训练组至少50%的肿瘤细胞出现PD-L1表达被作为截止点。验证组百分比至少为50%的患者的反应率为45.2%。而所有百分比至少为50%的所有的患者的无疾病进展中位生存期为6.3个月,但这些患者未达到总生存期的中位时间。
本研究由Merck资助:KEYNOTE-001临床试验国家编号NCT01295827;研究链接:Pembrolizumab for the Treatment of Non–Small-Cell Lung Cancer
MedSci注:这项研究确立后,未来会将免疫治疗配合传统的化疗或靶向治疗进行研究,以及能否从晚期的二线治疗推向一线治疗或维持治疗,以及将来是两种免疫治疗共同结合研究的可能。这些均值得拭目以待。而且KEYNOTE-001从命名来看,这将是一个庞大的、系列研究过程,未来将推动实体瘤的巨大进展!
免疫治疗的兴起,将来实体瘤的治疗打开新的思路。包括小分子的免疫治疗,多种免疫治疗结合,以及小分子免疫治疗结合CarT免疫细胞治疗,以及这些治疗与传统的经典化放疗,以及靶向治疗的优化结合,都是值得深入探索的。对于NSCLC而言,已经有漫长时间缺少对患者OS获益的研究了,免疫治疗成为新的期待。对于NSCLC治疗而言,不仅仅是PFS的延长,更应该是OS的延长。
原始出处:
Garon EB, Rizvi NA, Hui R, Leighl N, Balmanoukian AS, Eder JP, Patnaik A, Aggarwal C, Gubens M, Horn L, Carcereny E, Ahn MJ, Felip E, Lee JS, Hellmann MD, Hamid O, Goldman JW, Soria JC, Dolled-Filhart M, Rutledge RZ, Zhang J, Lunceford JK, Rangwala R, Lubiniecki GM, Roach C, Emancipator K, Gandhi L; KEYNOTE-001 Investigators.Pembrolizumab for the Treatment of Non-Small-Cell Lung Cancer. N Engl J Med. 2015 Apr 19.
小知识:癌症的免疫治疗
目前癌症的治疗途径和及其特点
1.手术治疗,针对局部肿瘤
2.放射治疗,转移性肿瘤,影响分裂细胞(骨髓细胞等),易产生抗性
3.化疗,转移性肿瘤,影响分裂细胞(骨髓细胞等),易产生抗性
4.靶向治疗,易产生抗性
5.免疫治疗,转移性肿瘤,不易产生抗性,毒性小
6.综合治疗
免疫系统在排斥肿瘤作用中的一些证据
1.肿瘤自然缩小和消失
2.原发肿瘤移除后,转移肿瘤会缩小和消失
3.化疗后,肿瘤缩小和消失
4.肿瘤内侵有淋巴细胞和巨噬细胞
5.有免疫抑制或缺陷的病人及老年人,癌症发生率高
引起肿瘤免疫反应的条件
1.肿瘤应表达外源抗原
2.肿瘤具有免疫性
3.病人应有免疫能力
肿瘤如何逃避免疫识别
1.肿瘤产生抑制细胞
2.分泌免疫抑制分子
3.肿瘤细胞表面抗原的表达减弱
4.肿瘤细胞表面MHC的表达减弱
5.肿瘤的一些激活T细胞的分子表达减弱(B7)
6.肿瘤的一些抑制T细胞的分子表达增强(PD-L1)
什么是肿瘤免疫治疗
利用人体本身的免疫系统来治疗肿瘤,它包括:1.激活患者本身的免疫系统,2.提供免疫系统中的一些成份来更有效地杀死肿瘤细胞
肿瘤免疫治疗的常见途径
特异性的免疫治疗:
单克隆抗体:
裸抗体(Avastin、Herceptin、Erbitux)结合抗体(ADC, Bi-specific 抗体)
肿瘤疫苗:
肿瘤细胞疫苗
肿瘤抗原疫苗 (MUC1, MAGEA3)
树突状细胞疫苗 (Sipuleucel-T (Provenge)-前列腺癌)
溶瘤病毒
非特异性的免疫治疗:
细胞因子或化合物 :
激活免疫活性T细胞 (白细胞介素 IL2,干扰素 )
抑制负调节活性T细胞 的免疫细胞 (Treg, MDSC)
免疫系统检查点阻断剂 :
CTLA-4(CytotoxicT lymphocyte antigen 4)-ipilimumab,又名Yervoy,3/2011US BMS)
PD-1(Programmed Death 1):nivolumab(Opdivo, 7/2014Japan,BMS);Keytruda (pembrolizumab;MK-3475, 9/2014 US, Merck)
免疫系统辅助激活剂(4-1BB, OX40, ---)
过继免疫细胞疗法 (NKs, LAK细胞疗法,TIL过继免疫)
CAR修饰T细胞 (ChimericAntigen Receptor modified T cells)-(anti-CD19, B细胞淋巴瘤)
在肿瘤微环境中T细胞,树突状细胞,肿瘤细胞和巨噬细胞间,配体 - 受体相互协同刺激和抑制的作用
Ott P A et al. ClinCancer Res 2013;19:5300-5309
CTLA-4和PD-1调控T细胞的不同反应-CTLA4 分管早期活,PD-1主要表达于有抗原记忆的T细胞。肿瘤细胞通过上调PD-1的配体B7-H1和B7-DC的表达来逃避T细胞对肿瘤的免疫反应
OttP A et al. Clin Cancer Res 2013;19:5300-5309
T细胞的调节反应是通过多种协同刺激和抑制的相互作用来实现的
1.T细胞对抗原的反应是通过T细胞受体识别的肽-MHC介导的,具特异性
2.膜结合配体B7家族能结合协同刺激受体也能结合协同抑制受体
3.CTLA-4和PD-1抑制性受体的靶向药物治疗是目前主要的临床重点
ipilimumab,又名Yervoy:Anti–CTLA-4单克隆抗体,FDA 批准3/2011 US,BMS
1.治疗晚期黑色素瘤,但需要注意免疫相关不良反应
2.单独或结合别的药物的临床试验的有非小细胞肺癌(NSCLC),小细胞肺癌(SCLC),膀胱癌,和转移性激素难治性前列腺癌,和晚期黑色素瘤的治疗。
3.会有更多的结合别的药物的临床试验
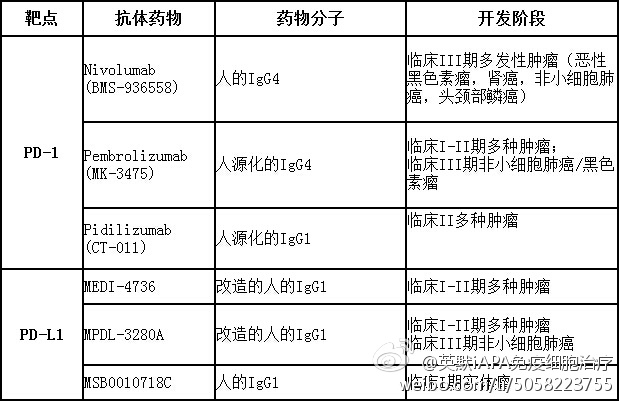
PD-1/PDL1免疫检查点抑制剂的临床开发
 Ipilimumab引起一小部分患者有持久的药效,但没有改变存活曲线的早期部分
Ipilimumab引起一小部分患者有持久的药效,但没有改变存活曲线的早期部分
用PD1或PD-L1抗体治疗有反应的肿瘤类型
黑色素瘤(Pembrolizumab于2014年9月通过美国FDA,用于不能手术切除或转移性肿瘤而且在ipilimumab/BRAF抑制剂治疗后无效的晚期黑色素瘤);肾癌;非小细胞肺癌;膀胱癌;头颈部肿瘤;淋巴瘤。
临床上利用PD-1通路阻断治疗肿瘤的一些问题
1.具预测性的生物标记物 (PDL1?---):哪些肿瘤可治疗?哪些患者可治疗?
2.肿瘤免疫治疗中抗性的产生
3.其它组合治疗?
4.对没有免疫浸润的肿瘤怎么治疗?
阻断CTLA-4和PD-1 / L 1两个免疫检查点来治疗癌症
1.Ipilimumab Nivolumab组合治疗显著延长了晚期黑色素瘤患者的生存期(2014ASCO)。
2.1年生存率为85%,现在进一步随访2年生存率为79% (2014ASCO)。
3.与每单个药物治疗相比,组合治疗也导致毒性增加。
4.3,4级副作用有58 /94例(62%),但是是可控和可逆的。
5.III期临床试验登记已经完成, 比较Ipilimumab Nivolumab与单独Nivolumab或Ipilimumab。
6.II期试验Nivolumab加上Ipilimumab比较单独Nivolumab。
其它与PD-1免疫检查点抑制剂的组合治疗
其他免疫协同抑制途径•TIM-3,LAG-3,氧酶
其他免疫激活途径合作或免疫途径•OX40,4-1BB,GITR,IL-2,IFN,IL-21,IL15
常规治疗
化疗,TKI,VEGF抑制剂
癌症疫苗
表观遗传治疗
代谢治疗
总之:
1.现代免疫治疗对很多癌症患者带来希望,有些产生持久的抗肿瘤反应 。
2.免疫治疗包括免疫检查点抑制剂的治疗跟常规疗法不同。
3.越来越多的数据表明免疫检查点抑制剂靶向PD-1/ PD-L1存在于多种肿瘤类型中。
3.目前正在进行的研究将有助于优化免疫检查点抑制剂用在不同肿瘤类型中。既可作为单独药物也可作为综合治疗的一部分。
肿瘤免疫治疗在中国也发展很快。
4.自行研发的免疫检查点抑制剂靶向治疗预计在2016和2017进入临床试验。(LiYan and Helen Chen 2014, Chinese Journal of Cancer)
5.Ipilimumab,Pembrolizumab和 Nivolumab也已在中国开展临床试验(胃癌, 肝癌和肺癌)。(LiYan and Helen Chen 2014, Chinese Journal of Cancer)
6.其他免疫治疗方法包括肿瘤疫苗,细胞因子,过继性T细胞治疗(例如 CAR-T细胞治疗)发展迅猛,开创了中国肿瘤免疫治疗的新时代。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Pembro#
49
#mAb#
25
#抗肿瘤活性#
27
#KEYNOTE#
40
#肿瘤活性#
40
#PE#
31
值得期待的疗法
104
#Pembrolizumab#
31
#晚期NSCLC#
0
精彩,知识点非常集中
132