PNAS:让抗癌药“歪打正着”的研发策略
2016-10-11 佚名 药明康德
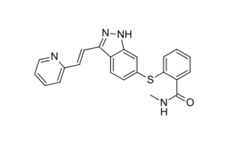
多年来,挪威卑尔根大学(University of Bergen)的Karl-Henning Kalland教授和Xisong Ke博士一直致力于研究肿瘤的演进,与在这当中发挥重要角色的细胞间信息传递机制,以找到可以阻断癌细胞间信息交流的潜在药物分子,从而避免癌细胞接受到促使其生长和扩散的信息。为此,他们对上千上万个化学特性已知的小分子进行了测试和筛选,其中既有从传统中药材中分离出的小分子,也有已



本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PNAS#
36
学习了,赞一个!
60
#研发#
25
#抗癌药#
21
继续关注!
47
谢谢分享!
55
好文章,受益
64
老药新用这是很好的思路
60
不错,也算一个比较有意义的思路
27